Research Article / Open Access
DOI: 10.31488/HEPH.168
Building a Comprehensive Advance Care Planning Approach in a Community Health System during COVID-19
Cynthia Anderson, MD*1, David Dekevich, MPH, MHA2, Ellen Schmitt, LCSW, CCM4, Elizabeth McCullough, MD3, Ellen Schmitt, LCSW, CCM4 , Mary Leen, DNP, ARNP5
1. Department of Radiation Oncology, Baptist MD Anderson, Adjunct Associate Professor, MD Anderson Cancer Center
2. Manager, Population Health Operations, Baptist Physician Partners, Baptist Health, 800 Prudential Drive, Jacksonville, FL USA 32207
3. Lead Physician, Ambulatory Palliative Care, Baptist Health, 800 Prudential Drive, Jacksonville, FL USA 32207
4. Advance Care Planning Consultant, Palliative Care, Baptist Health, 800 Prudential Drive, Jacksonville, FL USA 32207
5. Vice President, Clinical Operations, Baptist Physician Partners, Baptist Health, 800 Prudential Drive, Jacksonville, FL USA 32207
*Corresponding author:Cynthia Anderson, MD, Baptist MD Anderson Cancer Center, Department of Radiation Oncology,
Abstract
In response to the SARS-CoV-2 (COVID-19) pandemic, our community-based health system refocused efforts around advanced care planning (ACP). We rapidly pivoted from a population approach to a more narrow acute care focus for our critically ill, hospitalized patients. Methods: Our existing, physician-led, ACP Clinical Transformation Workgroup (CTW) created a “Comfort Measures and End of Life Symptom Management” order set, optimized workflows for completion of advance directive (AD) documents, and created a tiered palliative care staffing model in preparation for future surges of COVID-19 inpatient cases. Results: Three percent of patients admitted to our adult hospitals had at least one AD document in their electronic medical record (EMR). Six percent of patients treated for COVID-19 had at least one AD on file. The order set went live in August 2020 and it was activated for 30 patients. To complete AD documents, we developed a detailed flow chart to define the alternative decision-maker(s) and appropriate surrogate(s). The tiered palliative care staffing model has not been activated to date as we have not yet experienced an overwhelming inpatient volume. Conclusion: The SARS-CoV-2 pandemic afforded our CTW a unique opportunity to develop an acute strategy to address ACP-related issues. Slow adoption of some initiatives relate to the many concurrent healthcare changes occurring at our institution and the absence of an unmanageable surge thus far. We share our findings with a new level of system readiness, better prepared for the ongoing pandemic and potential unforeseen and disruptive healthcare events in the future.
Keywords: COVID-19, advance care planning, palliative care
Introduction
Advance care planning (ACP) is growing in importance in healthcare as an opportunity to align a person’s life goals and values with ongoing or future medical care [1]. Benefits of ACP include positive impacts on end-of-life care, decreased likelihood of futile treatments, and reduced medical costs [2,3]. Currently, the Centers for Medicare and Medicaid Services, through the Medicare Incentive Payment System (MIPS) and Alternative Payment Models (APM), include measures to track advance directive (AD) documents in the medical records of patients over age 65 [4]. In response, health care systems focused greater attention to this area of medical decision making to define patients’ wishes, provide goal concordant and quality care, and curtail escalating medical costs [5].
The SARS-CoV-2 (COVID-19) pandemic of 2020 created new challenges for healthcare systems to access or complete AD for inpatients receiving care. The elimination of outside visitors limited the ability to conduct family conversations for either shared decision making or to determine if a patient had already completed their AD [6]. Patients admitted for COVID-19 care, particularly those with underlying medical conditions, potentially faced rapid changes in health status which shortened the time to consider critical care or end-of-life (EOL) treatment options [7,8]. Furthermore, intubated or prone-facing patients experienced additional barriers to conducting goal-directed decision making conversations.
In addition, the changing models for healthcare delivery both compounded existing hurdles as well as created new opportunities for the ACP process. Limited availability of personal protective equipment (PPE) early in the pandemic constrained the number of patient-facing visits healthcare workers could provide [9]. A desire to limit staff exposure to COVID-19 both reduced the number of staff providing direct patient care and increased the likelihood that non-clinical staff would work remotely and, thus, be less available for ACP related conversations [10, 11]. The rapid development of telehealth medicine forced insurance providers to establish new policies for billing and coding, much of which was done at the discretion of each carrier, and therefore made variable the reimbursement for ACP [12, 13]. In addition, individual state policies vary in their allowance for remote completion of AD or for acceptance of conversations with family members across state lines for healthcare decision making [13]. Lastly, many health systems still rely on paper forms for consents and emergency healthcare directives and have limited development of computer based forms that allow for electronic signing or remote witnessing [15].
Baptist Health System of Northeast Florida (BHS) is a non-profit, community-based and locally governed health system. It includes four adult hospitals, one children’s hospital, over 50 primary care clinics, and multiple specialty service lines with over 1,000 physicians that serve a five-county area. It also encompasses Baptist MD Anderson Cancer Center, which is clinically and operationally integrated with MD Anderson Cancer Center in Houston. Baptist Physician Partners (BPP) is BHS’s clinically integrated network and accountable care organization (ACO).
In 2019, BPP convened a physician-led ACP Clinical Transformation Work Group (CTW). As a formally governed body within BPP, the ACP CTW reports to the Clinical Transformation Council, which in turn, reports to the BPP Board of Managers. Our original objective focused on developing pathways to access and/or complete AD documents across the care continuum including the ambulatory, hospital, and post-acute care settings.
Unexpectedly, the SARS-CoV-2 (COVID-19) pandemic of 2020 presented an urgent need to shift our focus to an acute care strategy. With no recent pandemic precedent, the ACP CTW worked from limited resources to develop a novel approach to address the needs of our patients and hospital care teams. Our CTW pivoted to three main objectives: create a standardized symptom management order set for critically ill patients, adopt new strategies to obtain and complete ADs for patients admitted to the hospital, and develop a system to bolster our inpatient palliative care (PC) resource pool in case of an overwhelming inpatient surge.
We share our findings as a reference tool for other healthcare systems working to modernize their approach to ACP and address urgent issues related to the COVID-19 pandemic.
Materials and Methods
Initial Efforts to Improve the ACP Process
Our CTW comprises a 43-member, interdisciplinary committee. Physician representation includes primary care, pulmonary and critical care, palliative care, cardiology, emergency medicine, hospitalist medicine, nephrology, neurology, medical oncology and radiation oncology. Additional support comes from BPP, health system administration, nursing, clinical informatics, spiritual care, bioethics, social work, ambulatory care coordination, pharmacy, and inpatient case management. Community participation includes Honoring Choices Florida®, a statewide initiative designed to integrate ACP into routine health care.
The CTW met weekly to develop a new, system-wide approach to ACP for all of our patients. In March 2020, Florida experienced a rise in cases of COVID-19 with an anticipated surge by June 2020. As BHS adjusted hospital preparation, the ACP CTW shifted focus.
Shifting Goals due to the COVID-19 Pandemic
Our first goal was to create a novel symptom management and end of life order set to promote palliation and accommodate a potentially large volume of need. Our prior model for acute and critical care symptom management relied on physicians to write orders for each patient based on individualized provider preference. This limited our ability to standardize and scale efforts across all four adult hospitals. The CTW developed the order set which our governing bodies reviewed and approved.
Secondly, the CTW created workflows to obtain and/or complete documents for patients whose ADs were not accessible in our electronic medical record (EMR). To update our process, we developed a new surrogate/health care proxy inpatient workflow that referenced Florida statutes regarding proxy and orally declared ADs. The CTW reviewed and approved the changes, created comprehensive education strategies, and held training workshops to educate our case management staff.
Lastly, the CTW approved a unique palliative care tiered-triage model to increase resources in preparation for a surge of COVID-19 inpatient admissions. In 2011, BHS contracted with a community resource to develop a full-time, inpatient PC service for our hospitals. Physicians licensed in PC, advanced practice registered nurses, licensed clinical social workers (LCSW), and chaplains comprise the team. In addition, our two larger adult hospitals have a 10-room inpatient hospice unit specializing in complex symptom management and end of life care.
The early stages of the pandemic were projected to tax resources in the inpatient setting while simultaneously freeing other providers due to a reduction in clinic hours and the cancelation of elective procedures. In April 2020, BHS administration sent an email survey to all physicians and staff to define their areas of expertise as well as an option to volunteer. Those who volunteered were placed in a pool from which emergency responders could be drawn.
Because of the frequent overlap in palliative care and oncology services, those who volunteered from Baptist MD Anderson Cancer Center were assigned to the inpatient palliative care team. Several radiation oncology providers hold a specialty certification in palliative medicine. These providers and the PC team collaborated to develop a daily emergency response plan to meet the anticipated increased demand for inpatient services.
Results
Medication order set
Our CTW developed the “Comfort Measures and End of Life Symptom Management” (Figure 1) order set, a complex symptom management tool that included a wide-range, multispecialty perspective. We employed clinical standards of care based on recommendations from CTW physician members. Medication orders addressed common symptoms including pain, agitation, excessive secretions, nausea, fever, and constipation. It also included selections for diet choice, patient positioning, respiratory care, and placement of consults. New to this order set was the availability of complementary services such as ethics, the integrative care service, and spiritual care. BHS implemented the order set on August 4, 2020. From initiation through February 28, 2021, the order set was activated for 30 patients, seven of whom had COVID-19 (Table 1).
AD Documents for hospitalized patients
To improve the inpatient care team’s ability to identify a HCS or proxy for patients, the ACP CTW updated the existing process for defining the alternative decision-maker(s). The new document included a detailed flowchart and supplemental checklist (Figure 2). It referenced Florida Statute 765.401 to identify the patient’s health care proxy for those who did not have capacity or legal documentation in the EMR (16). Acceptable sources of health care decision maker documentation included primary care and specialty clinics, skilled nursing facilities, identifiable family members, or individuals as defined by Florida Statute 765.202.
Table 1.Inpatient Comfort Care PowerPlan Use by Diagnosis from August 4, 2020- February 28, 2021 Source: Cerner Millennium
| MED Comfort Measures and End of Life Symptom Management Order Set | |
|---|---|
| Condition | Number of Times Ordered |
| Alcohol Abuse or Dependence | 1 |
| Atrial Fibrillation | 1 |
| Bowel Obstruction | 2 |
| Coronavirus (COVID-19) Disease | 7 |
| Dementia | 1 |
| Intracranial Hemorrhage | 1 |
| Liver Cancer | 1 |
| Pancreatitis | 1 |
| Pneumonitis | 1 |
| Pneumothorax | 1 |
| Pulmonary Embolism | 1 |
| Renal Failure, Acute | 3 |
| Respiratory Failure | 3 |
| Sepsis, Other | 6 |
| TOTAL | 30 |
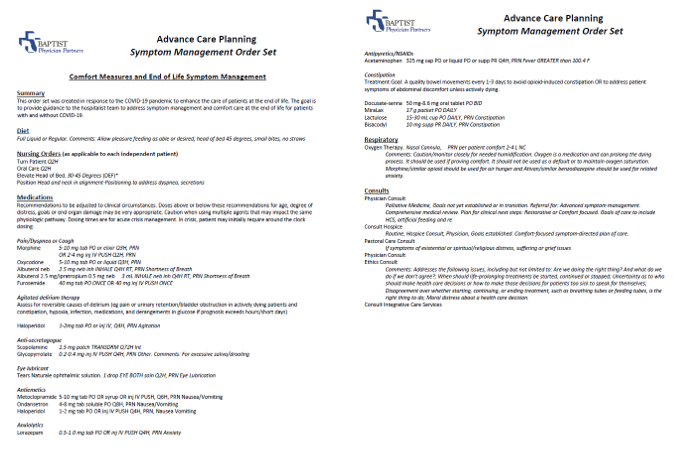
Figure1:Comfort Measure and End of Life Symptom Management Order Set in Cerner Millennium
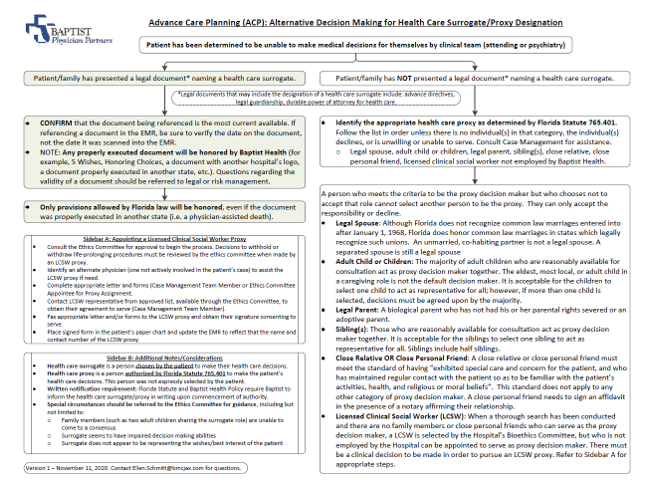
Figure2:Alternative Decision Making for Health Care Surrogate/Proxy Designation
Table 2.Unique patients (age ≥18) who had as least one advance directive document in their inpatient electronic medical record, March 1, 2020 to February 28, 2021. Source: Cerner Millennium
| Unique Patients COVID-19(+) | COVID-19(+): At Least One AD Doc | % COVID-19(+): At Least One AD Doc | Unique Patients COVID-19(-) | COVID-19(-): At Least One AD Doc | % COVID-19 (-): At Least One AD Doc | TOTAL Unique Patients | TOTAL: At Least One AD Doc | % TOTAL: At Least One AD Doc | |
|---|---|---|---|---|---|---|---|---|---|
| Beaches | 593 | 87 | 14.7% | 9,067 | 317 | 3.5% | 9,660 | 404 | 4.2% |
| Jax | 1,871 | 95 | 5.1% | 35,381 | 1,410 | 4.0% | 37,252 | 1,505 | 4.0% |
| Nassau | 339 | 14 | 4.1% | 6,690 | 94 | 1.4% | 7,029 | 108 | 1.5% |
| South | 1,953 | 99 | 5.1% | 30,183 | 827 | 2.7% | 32,136 | 926 | 2.9% |
| Total | 4,756 | 295 | 6.2% | 81,321 | 2,648 | 3.3% | 86,077 | 2,943 | 3.4% |
If patients were able to communicate while in COVID-19 isolation rooms, we conducted virtual conversations via tablets to limit staff members’ viral exposure and conserve PPE. ACP staff assisted patients to declare and complete ADs orally, as allowed by Florida Statute 765.204. Completed ADs were witnessed and uploaded to the patient’s medical record.
From March 1, 2020 to February 28, 2021, 3.4% of the 86,077 unique patients admitted to our adult hospitals had at least one AD document scanned into their medical record. AD documents included living wills, health care surrogate (HCS) designations, durable DNRs, and health care powers of attorney. Table 2 displays a breakdown of patients that had at least one advance directive in their EMR during this timeframe. Of note, 6.2% of all patients treated for COVID-19 had at least one AD on file.
Tiered-triage model
The tiered-triage model was developed in collaboration between PC and Baptist MD Anderson Cancer Center radiation oncology leadership (Figure 3). We built two emergency preparedness clinical pathways to activate when care team demand exceeded supply.
Triage Pathway A included inpatient social workers (including LCSWs), nurses, and spiritual care staff. Assigned responsibilities included patient and family contact, information gathering, and psychosocial counsel. It was activated upon need in late July 2021. Triage Pathway B included physicians and advance practice partners. Assigned responsibilities included patient consult coordination, symptom management, and goals of care discussions. The level of assistance provided escalated through several tiers, with increasing resources devoted as required. Tiers were used to efficiently integrate our oncology providers into our fast-paced inpatient PC service during a time of high volume and uncertain clinical circumstances.
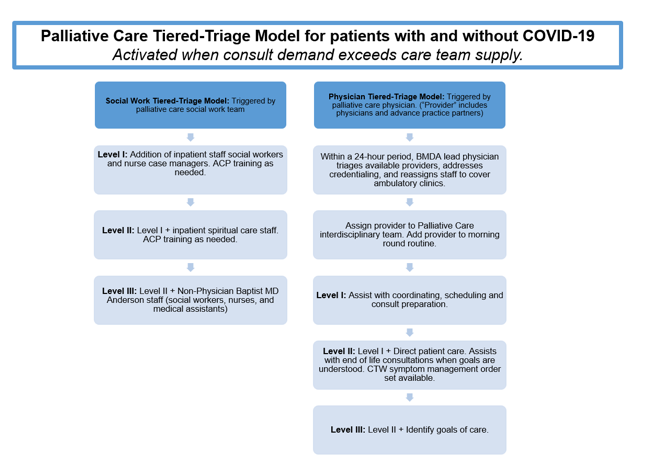
Figure3:Palliative Care Team Tiered-Triage Model
To acclimate providers to the complexity of inpatient palliative care, we created rapid, informal training. Content included an overview of the PC consultative role including symptom management, review of medical comorbidities, defining goals of care, identifying decision-making obstacles, and respecting patients’ psychosocial, religious and existential preferences. The model included weekly reassessments driven by metrics including inpatient PC consult volume and current service census.
Discussion
ACP is a vital tool to provide concurrently the care patients want while preserving the finite resources others may need. It is gaining more attention in healthcare systems as an opportunity to deliver goal-concordant care, improve patient quality of life, decrease decisional conflict, and reduce futile medical interventions and costs [17]. The selection of ACP as one of the reform goals of MIPS/APMs has elevated the need to complete ADs and make them available in EMRs. Documenting goals of care incentivizes systems to address widespread variation in practice, quality, and cost. As ACOs evolve to risk-bearing models, they seek to improve advanced illness and end of life care while ensuring efficient use of health care services [18,19].
The COVID-19 pandemic has magnified the importance of addressing ACP decisions [20,21]. The pandemic has resurfaced the long-standing ethical dilemma of resource rationing in times of medical crisis and shortage. Hospitals have faced insufficient inpatient beds, medical supplies, or available staff, increasing overall system duress [22,23]. Many healthcare systems have, therefore, seen the pandemic as opportunity to improve and adapt their ACP process as well. Furthermore, establishing goal-concordant care prior to urgent need has been cited internationally as a component of protecting the human rights of frail medical populations, who had higher rates of infection from COVID-19 [24].
Ongoing efforts continue in medical education to normalize these conversations for medical staff and ease hesitation about addressing AD as a perceived sensitive topic [25-27]. Additionally, Curtis et al. highlighted scalable process improvements to solicit and proactively complete ACP in vulnerable adults prior to a time of crisis or worsened infirmary. This included decisions for advance cardiac life support and/or DNR orders [28]. Liberman et al. described a successful emergency department program to complete the ACP process remotely with family members of patients who were too ill to participate in their decision own making. The creation of a nurse-led 24 hour phone line allowed for the majority of their participating patients to complete goals of care through telephone conversations [10].
Perhaps one of the most successful efforts in developing a remote ACP program has been WellSpan Health. This eight hospital healthcare system in Pennsylvania began improving their ACP process in 2014 and increased training to augment available staff during the pandemic. Analysis of their efforts demonstrated that patients who either had completed or were able to complete ACP during hospitalization were less likely to be admitted to the intensive care unit and incurred 25% lower medical costs, despite having elevated medical acuity [11].
BHS’s progressive focus on population health through BPP allowed our work on ACP to begin well before the pandemic reached Florida. Eventually, it required rapid reorganization of our CTW’s tools and initiatives. Our robust, collaborative relationship between physicians and administration allowed us to devote significant resources to craft the three pillars of our CTW’s COVID-19 response: a medication/intervention order set for global symptom management, a process for completing/obtaining AD’s and proxy assignments, and a tiered-triage plan to best utilize staff during a surge.
The medication order set was a request from the intensive care unit (ICU) team to ensure these interventions were not limited in scale during times of heavy patient volume. Although it had nominal initial use, we anticipate increased utilization with future COVID-19 surges. The intense focus of providers on direct patient care may have narrowed the bandwidth to incorporate new initiatives. In addition, at the time of our preliminary analysis, we had not experienced an overwhelming surge. With new variants of COVID-19 circulating, we are now facing a considerable volume increase. We plan to update our results at the next interim analysis.
Nationwide, approximately 18-36% of adults have at least one completed AD and hospital systems report about 20% of patients over age 65 have retrievable documents in their EMR [29,30]. Our model draws attention to our system-wide deficit; less than 5% of our patients have accessible ACP-related documents. The low availability of ADs in our inpatient EMR may be due, in part, to the disparate solutions used by our hospitals and outpatient clinics. This likely limited access to ACP documents and prevented accurate calculation. Due to the severity of disease caused by COVID-19, it was imperative that critical care providers can easily access AD documents in a timely manner. We are adopting a single, integrated EHR, which will address the disparity of having multiple EMRs across our health system’s care continuum. Furthermore, we anticipate staff training and use of tablets will improve the operational process of AD completion as noted in other institutions [31,32]. Additional challenges included patients unable to communicate verbally due to health status, visitation restrictions that limited access to alternative decision makers, and a desire to limit staff’s infectious exposure and use of personal protective equipment (PPE).
Related to PC staffing, COVID-19 created an unprecedented set of circumstances. Ambulatory clinics experienced a sharp decline in patient volume concurrent with an imminent threat for a hospital surge. To our knowledge, this is the first time an outpatient oncology service volunteered to work alongside palliative care colleagues to provide non-oncologic care. Considered variables included team staffing, consultation volume, COVID-19 daily admission rates and projections, ED holding and ICU communications. To date, triage pathway B has not been activated, but it remains available and will stand as a uniquely collaborative effort.
Future Directions
We focused on three foundational tenets with a goal for future integration and expansion. We will continue to promote and refine our order set with the aim of universal accessibility and increased utilization. Long term planning may include targeted patient surveys to assess symptom management impact versus control. Secondly, ACP is increasingly visible in the health system for both the patient and the clinician. We are migrating to a new EMR in 2022, which will positively impact standardization and document obtainability. In addition, ACP penetrance into such areas as citizenship metrics, core competencies and our alternative payment models defines it as a rising cornerstone of quality improvement and patient care. Lastly, we look toward future collaboration with and between our Palliative Medicine and Oncology colleagues. Though patient volume has now equalized across the inpatient and outpatient settings, this last surge saw open conversation for a modified and targeted triage plan. No matter the impetus, we anticipate this clinical deliberation will recur whenever additional inpatient resources may be beneficial.
Conclusion
We share our work to serve as a reference for other health care systems building a comprehensive advance care planning and supportive palliative care model. The pandemic intensified this need, and although in the early stages of implementation, theoretically, this model is replicable and scalable.
The need for ACP inclusion into medical decision-making continues to grow in universal importance. The pandemic magnified weaknesses in our ACP operational and clinical processes. It redefined and uncovered areas of opportunity even as it ravaged families and health systems. We have a bolstered ACP initiative that continues to grow in scope and we commit to overcoming our long-standing systemic fault lines. In this regard, perhaps COVID-19 can leave us better than it found us.
Disclosure and Conflict of Interest
The authors have no conflicts of interest to disclose. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
1. Hall A, Rowland C, Grande C. How Should End-of-Life Advance Care Planning Discussions Be Implemented According to Patients and Informal Carers? A Qualitative Review of Reviews. J Pain Symptom Manage 2019; 58:311-335.
2. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The Effects of Advance Care Planning on End-of-Life Care: a Systematic Review. Palliat Med. 2014;8:1000-25
3. Houben J, Spruitt HMA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of Advance Care Planning: a Systemic Review and Meta-analysis. J AM MedDIr Assoc. 2014;7:477-438.
4. Center for Medicare and Medicaid Services. Merit-Based Incentive Payment System Clinical Quality Measures Advance Care Planning. 2020.
5. Bond WF, Kim M, Franciskovich CM , Weinberg JM, Svendsen JD. Advance Care Planning in an Accountable Care Organization Is Associated with Increased Advanced Directive Documentation and Decreased Costs. J Palliat Med. 2018;4:489-502.
6. Bender M, Huang KN, Raetz J. Advance Care Planning During the COVID-19 Pandemic. J Am Board Fam Med. 2021;34(Suppl):S16-S20.
7. Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ. Epidemiology, Clinical Course, and Outcomes of Critically Ill Adults with COVID-19 in New York City: a Prospective Cohort Study. Lancet. 2020;395(10239):1763-1770.
8. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N Engl J Med. 2020; 21;382(21):2012-2022.
9. Cohen J, Rodgers YVM. Contributing Factors to Personal Protective Equipment Shortages during the COVID-19 Pandemic. Prev Med. 2020; 141:106263.
10. Liberman T, Roofeh R, Chin J, Chin K, Razack B, Aquilino J, Herod SH, Amato T. Remote Advance Care Planning in the Emergency Department During COVID-19 Disaster: Program Development and Initial Evaluation. J Emerg Nurs. 2021;30:S0099-1767(21)00252-X
11. Bhatia V, Geidner R, Mirchandani, Huang, Y, Warraich, H. Systemwide Advance Care Panning Durign the Covid-19 Pandemic: The Impact on Patient Outcomes and Costs. NEJM Catalyst Innovations in Care Delivery. 2021;2:9.
12. Martinez KA, Rood M, Jhangiani N, Kou L, Rose S. Patterns of Use and Correlates of Patient Satisfaction with a Large Nationwide Direct to Consumer Telemedicine Service. J Gen Intern Med. 2018;33(10):1768-1773.
13. Slightam C, Gregory AJ, Hu J, Jacobs J, Gurmessa T. Patient Perceptions of Video Visits Using Veterans Affairs Telehealth Tablets: Survey Study. J Med Internet Res. 2020;22(4):e15682.
14. Fu CJ, Agarwal M, Estrada LV, Murali KP, Quigley DD. The Role of Regional and State Initiatives in Nursing Home Advance Care Planning Policies. Am J Hosp Palliat Care. 2021;38(9):1135-1141.
15. Keesara S, Jonas A, Schulman K. Covid-19 and Health Care's Digital Revolution. N Engl J Med. 2020;382(23):e82.
16. State of Florida Statutes Advance Directives 2020.
17. Gabbard J, Pajewski NM, Callahan KE, Dharod A, Foley KL. Care Planning for Vulnerable Older Adults in an Accountable Care Organization: A Randomized Clinical Trial. JAMA Intern Med. 2021;3:361-369.
18. Gabbard J, Pajewski NM, Callahan KE, Dharod A, Foley KL. Advance Care Planning for Vulnerable Older Adults within an Accountable Care Organization: Study Protocol for the IMPACT Randomized Controlled Trial. BMJ Open. 2019;9:1-8.
19. May P, Normand C, Morrison RS. Economic Impact of Hospital Inpatient Palliative Care Consultation: Review of Current Evidence and Directions for Future Research. J Palliat Med. 2014;9:1054-1063.
20. Sultan H, Mansour R, Shamieh O, Al-Tabba' A, Al-Hussaini M. DNR and COVID-19: The Ethical Dilemma and Suggested Solutions. Front Public Health. 2021;9:1-7.
21. Sinclair C, Nolte L, White BP, M Detering K.Sinclair C. Advance Care Planning in Australia during the COVID-19 Outbreak: Now More Important than Ever. Intern Med J. 2020;8:918-923.
22. US Department of Health and Human Services Office of Inspector General. Hospital Experiences Responding to the COVID-19 Pandemic: Results of a National Pulse Survey. 2020; 23–27.
23. Emmanuel EJ, Persad G, Upshur R, Thome B, Parker M. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N Engl J Med. 2020; 382:2049-2055
24. Gilissen J. International COVID-19 Palliative Care Guidance for Nursing Homes Leaves Key Themes Unaddressed. J Pain Symptom Manage. 2020:2, e56-69.
25. Wing C, Chan H, Hiu N, Ng Y, Chan YL. A Systematic Review of the Effects of Advance Care Planning Facilitators Training Programs. BMC Health Serv Res. 2019;19:362.
26. “Basic Advance Care Planning Course.” www.wsma.org
27. “Building Physician Skills in Basic Advance Care Planning.” www.capc.org
28. Curtis JR, Kross EK, Stapleton RD.Curtis JR. The Importance of Addressing Advance Care Planning and Decisions About Do-Not-Resuscitate Orders During Novel Coronavirus 2019 (COVID-19). JAMA. 2020;18:1771-1772.
29. US Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability and Aging. Advance Directives and Advance Care Planning.
30. Yadav KN, Gabler NB, Cooney E, Kent S, Kim J. Approximately One In Three US Adults Completes Any Type Of Advance Directive For End-Of-Life Care. Heath Aff. 2017;7:1244-1251.
31. Walter KL, Joehl HE, Alrifai T, Varghese TG, Tyler MJ. A Quality Improvement Initiative to Increase Completion and Documentation of Advanced Directives in the ICU at a U.S. Community Teaching Hospital. Crit Care Exlpor. 2021;5:1-8
32. Portz JD, Brungardt A, Shanbhag P, et al. Advance Care Planning Among Users of a Patient Portal During the COVID-19 Pandemic: Retrospective Observational Study. J Med Internet Res. 2020;8:1-11.
Received: October 05, 2021;
Accepted: October 21, 2021;
Published: October 26, 2021.
To cite this article : Anderson C, Dekevich D, Schmitt E, et al. Building a Comprehensive Advance Care Planning Approach in a Community Health System during COVID-19. Health Education and Public Health. 2021; 4:3.
© 2021 Anderson C, et al.
