Research Article / Open Access
2020; 3(6): 357– 364 doi: 10.31488 /HEPH.156
Developing A Community-Based Tobacco Control Intervention to Reduce Secondhand Smoke Exposure Among Children and Promote Smoking Cessation Among Household Members in Rural China: a Qualitative Study
Zixian Pan1, Xiao Xiao Chen2, Pinpin Zheng3, Jingyi He3, Wei Hao2, Haijiang Lin2, Abu S Abdullah1,4,5*.
1. Global Health Research Center, Duke Kunshan University, Jiangsu 215347, China.
2. Taizhou City Centers for Disease Control and Prevention, Taizhou, Zhejiang 318000, China
3. Department of Preventive Medicine, School of Public Health, Fudan University, Shanghai 20032, China
4. Duke Global Health Institute, Duke University, Durham, NC 27710, USA
5. Boston University School of Medicine, Boston Medical Center, Boston, Massachusetts 02118, USA
*Corresponding author: Abu S Abdullah MD., MPH., PhD., FFPH; Global Health Research Center, Duke Kunshan University, 8 Duke Avenue, Kunshan, Jiangsu Province, 215347, China.
Abstract
Background: Little is known about the smoking behaviors and household smoking practices among rural population in developing countries, and among the Chinese rural residents.The purpose of this study is to explore the perception of a tailored health education intervention, smoking hygiene intervention (SHI), to address secondhand smoke (SHS) exposure reduction and promote smoking cessation in rural Chinese households.Method:We conducted three focus group discussions (FGDs) of 18 residents in rural Taizhou. FGDs were audiotaped, transcribed and analyzed thematically.The FGDs guided the tailoring of all intervention materials for use by rural Chinese population in a subsequent randomized controlled trial. Results: Participants considered the proposed SHI intervention to reduce children’s SHS exposure and promote smoking cessation in adults, in general, is appropriate for rural Chinese. Participants provided suggestions on the content and design of the intervention, which are relevant to improve the acceptability and usability of the SHI intervention.These aresummarized under three major themes: (1) perceptions about smoking and SHS exposure, (2) perceptions about smoking cessation and SHS exposure reduction intervention, and (3) design considerations (i.e. contents and delivery) of the SHI.Conclusion: This qualitative study in rural Chinese household members provides insights about the need and delivery of a community-based intervention to reduce children’s SHS exposure and promote smoking cessation in the households of rural China. The findings informed the development of a revised SHI model for use by the rural Chinese household members, which is now being evaluated in an ongoing randomized controlled trial.
Keywords:Secondhand smoke; children;tobacco;tobacco control intervention; rural China
Introduction
Exposure to secondhand smoke (SHS) among young children has been a major public health concern [1]. SHS is the combination of smoke emitted from the burning end of a cigarette or other smoked tobacco products and the smoke exhaled from the lungs of smokers [2]. A large and accumulating body of scientific evidence has confirmed the negative impacts of SHS exposure on infant and child health. Young children and infants who are exposed to SHS have a higher risk for respiratory disorders, including asthma, bronchitis, and pneumonia [3]. Globally, exposure to SHS is responsible for an estimated 600,000 deaths and almost 11 million disability-adjusted life-years (DALYs) per year; and among all cases, children made up over a quarter of deaths and over half of DALYs associated with SHS exposure [4]. With an estimated 301 million current smokers in 2010 [5], the trends in tobacco consumption continued to increase in China. More than 90 percent of the Chinese smokers reported smoking in public spaces [6], resulting in 740 million non-smokers passively exposed to SHS, including 180 million children under 15 years old [7]. Particularly, smoking prevalence was higher among rural residents (29.8%), compared to urban residents (26.1%) [8]; while a national survey in 2013 revealed that the awareness of health risks related to SHS exposure was 60.0% in rural areas, lower than the rate in urban areas (77.0%) [9]. The high rates of smoking and low awareness of health hazards from smoking among the rural public have contributed to severe SHS exposure (68%) among nonsmoking children (aged 0-18) in rural areas [10].
Young children are more vulnerable to being exposed to SHS. An estimated 40–50% of the world’s children are regularly exposed to SHS, primarily by being around smoking parents and/or other household members [4]. As homes havebecomethe predominant location for children’s exposure to SHS [11], caregivers’ decisions regarding smoking behaviors at home strongly influence the SHS exposure levels of young children. The American Academy of Pediatrics (AAP)has recommended proper smoking hygiene (i.e. smoking away from the immediate environment of infants and children) to eliminate children’s exposure to SHS and improve child health[12].
Promoting household smoking bans is a prominent strategy for protecting the health of young children [13]. Although Cramer et al. [14]suggested developing community programs that helped eliminate exposure to SHS, there were few community-level interventions [15].
A previous study has shown the success of implementing a SHS exposure reduction intervention in Chinese urban areas (i.e. Shanghai) by engaging community health centers [16]. In the rural setting, village doctors (VDs) are responsible for health education and promotion [17, 18]; and there were a few community-based health intervention programswhile most of them focused on non-communicable diseases (NCDs) prevention or management. Thus, little is known about the smoking behaviors and household smoking hygiene practices among Chinese rural residents; andit is not clear whether a smoking hygiene intervention (SHI) that was proven effective among the urban households [16] will be acceptable among rural residents.
Qualitative research, as well as providing important insights into processes of intervention development, is a good way to involve users by allowing for a wider range of views to be canvassed and systematically incorporated into the intervention [19]. The degree to which an intervention can be adapted, tailored, and refined to meet local needs (i.e., the needs of rural Chinese) is a core component of implementation [20]. Therefore, the purpose of this study is to explore, through qualitative methods, the perception of a tailored health education intervention, smoking hygiene intervention (SHI) [16], to address tobacco smoke exposure reduction and promote smoking cessation in rural Chinese households. The “SHI” (see Methods section for details) was proven effective to reduce SHS exposure among children in urban Chinese households [16], but not tested for rural Chinese population.
Methods
SHI is designed to address SHS exposure issuesaround children by improving household smoking hygiene practices. Smoking hygiene practices focuses on the following aspects: 1) keeping the child away from household members’ and other visitors’ smoke, 2) avoidance of smoking in closed areas near the child, and 3) enforcing a smoke-free policy at home. The intervention is conceptualized on the basis of the protection motivation theory(PMT) developed by Rogers[21]. The counseling follows a patient centered approach, which means that the counselor engaged the households in a discussion about smoking and SHS exposure to the child in a nonthreatening manner and engage the household members in making decisions about the counselor’s recommendations for SHS exposure reduction and/or quit smoking [16].
Study setting
The study was conducted in Taizhou, located at central Zhejiang province. Zhejiang is an economically developed region in eastern China. In 2017, the GDP per capita of Taizhou was ¥72,912 (~10,500 USD) [22]. High SHS exposure at home (60.9%) and in public (65.3%) was reported in Zhejiang [23]. With the aim of building a health-first and people-oriented culture, the local Centers for Disease Control (CDC) has implemented a number of public health campaigns to provide knowledge about tobacco among the public and promote a non-smoking social atmosphere [24].Rural population accounted for 37.8% of the total population of Taizhou [22]. The terrain of Taizhou is characterized by mountains which contributes to the scattered distribution of villages. In rural areas, the major economic activity is agriculture.
Participants & recruitment
Eighteen residents from local communities in Linhai (a county-level city in Taizhou) participated in the focus group discussions (FGDs).The eligibility criteria for the FGD was: 1) parent (father or mother) or care giver of a child aged 5 years or below; 2) residents of the local rural community; 3) having at least one family member who was a smoker; 4) being a smoker (currently smoke at least 1 cigarette daily) or ex-smokers (who smoked in the past but now had quit) or ever-smoker (who tried cigarettes on few occasions); or non-smoker. Participants were recruited via an online poster shared on WeChat Subscribed Articles (a Chinese social media platform), whereby people could register for the FGDs.A coordinator from the local Centers for Disease Prevention and Control (CDC) assisted with the recruitment process.
Procedure
The FGDs were conducted in May 2018. Written informed consent was obtained from each participant before the discussions started. FGDs were held on a designated meeting room of Linhai CDC. The same researcher with a notetaker moderated all three sessions. Each discussion lasted for approximately 60 minutes. The moderator followed a semi-structured interview guide. The FGDs were conducted in Mandarin Chinese and were recorded by two digital voice recorders. To compensate participants for their time, a cash amount of 100 RMB (~15 USD) was given to each participant.
The semi-structured interview guide used for FGD comprised of two parts: i) patterns of smoking behaviors and smoking hygiene practices in the households and community; and ii) discussions about the content and delivery format of the proposed smoking hygiene intervention (SHI). Participants were first asked about: (for smokers only, either current or past) the reasons for smoking, quitting, or relapsing (if ever); knowledge about harms of smoking and SHS; concerns about children’s exposure to SHS; barriers to smoking cessation and establishing smoke-free regulation at home. Then, the participants discussed the design, components and delivery format of an existing SHI which was previously used among the urban population in Shanghai[16] and provided insights about how this SHI could be tailored to make this more relevant for rural population.
The study was approved by the ethical review boards at Duke Kunshan University (No: 2018PAN007).
Analysis
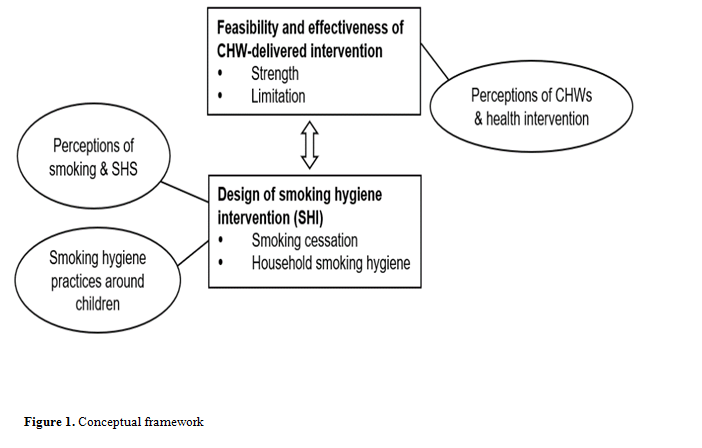
Audio recordings for both FGDs were transcribed verbatim, supplemented by notes taken during the discussions. Transcripts were coded by the author (ZP) using NVivo 12 analytical software. Structural codes generated from the interview guides were first applied to segment the text, with input from the research supervisor (ASA)and other researcher (JH). Transcripts were read carefully to mark evidence that supported the findings and check for any missing message. To answer the research questions, a conceptual framework (Figure was created. The coding process was conducted in English by using transcripts in the source language of Mandarin Chinese in order to retain the original meaning. Key themes were identified through the process of coding. Quotes presented in the results section were extracted and translated into English verbatim by the author (ZP). Selected excerpts from focus groups were translated into English for reporting and backtranslated for checking by the researchers who were bilingual (Mandarin and English).
Results
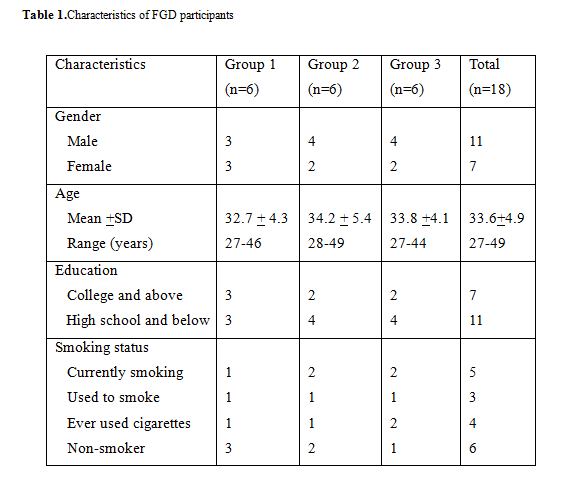
We recruited 18 participants (parents of young children residing in the target rural community) for three FGDs (Table 1).The participants were divided into three groups based on their order of agreement and time availability. All,but one, of the participants who had eversmoked were males, includingfivecurrent smoker, three ex-smokers (who smoked in the past but now had quit), and threeever-smokers (who tried cigarettes on few occasions); one ever smoker was female. All the six non-smokers were female, but all had a smoker household member residing in the same house.
Themes identified from the analyses
Thematic analysis identified three major themes from the data. These included:(1) perceptions about smoking and SHS exposure, (2) perceptions about smoking cessation and SHS exposure reduction intervention, and (3) suggestions for modifying (i.e.content and delivery format) of the proposed SHI. These themes are described below, supplemented by statements extracted from participants’ narratives.
Perceptions about smoking and SHS exposure
Under this theme, we identified three subthemes: a) attitudes towards smoking around children, b) adoption of smoking hygiene practices among smoker households, and c) perceptions of community-based SHI.
Smoking was perceived as a common practice among rural residents. All the participants in the FGDs reported knowing a few smokers. All thought that cigarette smoking is widely accepted within the society and cigarettes are still distributed during social activities, such as wedding parties. Few argued that in business occasions, cigarettes are shared as a way of showing kindness.
“If you live in rural areas, everyone around you smokes so that you are viewed as weird if you do not smoke.”
However, with a bad impression of smoking, harmful effects to health and unpleasant smell, smokers were sometimes unwelcomed, especially by females. Nonsmokers in the FGDs showed negative attitudes towards smoking behavior and smokers.
“I have a friend who smokes while his girlfriend [who dislikes smoking] asked him to quit. He did not listen and therefore, they broke up.” (Ex-smoker, male, 48)
Concerns about being exposed to SHS
The concept of SHS was widely known among the participants. Most participants in the FGDs realized the fact that exposure to SHS was bad to health but they were not clear about how serious the consequences might be. Nonsmokers were concerned about being exposed to SHS and believed their exposure to SHS would cause sickness. A participant (nonsmoker, female, 36) claimed SHS was even more harmful than smoking. Several participants reported they felt uncomfortable when people were smoking around them.
“I cannot tolerate it if more than one person is smoking; my eyes hurt.” (Female, non-smoker, 43)Several parents were more cautious about their child’s exposure to SHS.
“If I take my child out for dinner and there is someone smoking around, I will remind him of not smoking in the presence of kids, … if he does not listen I will move to another seat.” (Female, non-smoker, 33)
Perceptions about smoking cessation and SHS exposure reduction intervention
Under this theme, we identified three subthemes: a) attitudes towards smoking around children, b) adoption of smoking hygiene practices among smoker households, and c) perceptions of community-based SHI.
Attitudes towards smoking around children
Participants, in general,realized the fact that smoking around children is harmful. However, when discussed about the specific illnesses related to SHS exposure few participants did not know that SHS exposure could cause respiratory illnesses (5 out of 18) or intellectual impairment (8 out of 18).
“I do not agree that SHS exposure causes many health problems (shortness of breath or pneumonia). For example, in my next-door apartment, no one smokes cigarettes, but I see their daughter is always cough/sick and they go to hospital often; ………In contrast, my father and I smoke often at home, but my son is seldom sick…” (Smoker, Male, 41).Another ex-smoker (male, 44) said, “my friend is a heavy smoker, but his son is the 1st in the class”.
Adoption of smoking hygiene practices among smoking households
Smoking restrictionswithin the households were commonly adopted in the households of most of the participants. Generally, smoking was restricted in the home when children were at present. To care for children, most smokers would voluntarily go outside to smoke. When someone smoked inside the house, mainly visitors, most participants would open the window for ventilation. In some families, smoke-free regulations were established. For example, smoking was only allowed on the balcony; or smoking was not allowed in the bedroom.
“Our child was taken care of by my father-in-law when the child was young…he [my father-in-law] was cooperative – he did not smoke at home; he would smoke outdoors.” (ex-smoker, male, 31)
However, one mother (nonsmoker, 43) complained that her husband and father would smoke within the house regardless of the child’s presence, especially after dinner.
Perceptions of community health worker deliveredSHI
SHI to support household smoking hygiene
Participants in the FGDs, mainly nonsmoking mothers, suggested it was difficult to establish complete smoking bans in the home as they were unable to stop elders and visitors from smoking. Older generations might not recognize the negative impacts of SHS on health of others and they smoked whenever they wanted, ignoring the presence of young children. Additionally, participants thought it would be impolite to restrict visitors to smoke. Mothers would usually take the child away or open windows for ventilation, instead of asking the smoker to put out the cigarettes. “If the elder comes, …, he certainly needs to smoke; we know his addiction and would allow him to smoke… we just tell the child to go to another room” (A mother of a 7-year-old, 34) SHI to support smoking cessation
Participants identified several challenges for smokers to quit:low motivation, addiction to tobacco, and lack of quitting support.Most (4 out of 5) smokers did not perceive or believe risks related to smoking. Even though they heard a lot about adverse health effects of smoking and smoking-associated diseases, they did not think the misfortune will happen to them, unless they finally get sick.“Addiction to cigarettes” was frequently referred to when discussing smoking cessation barriers. Smokers thought it was impossible for them to quit smoking, especially for those who had smoked for a long time.Besides, it was mentioned once a smoker relapsed, their addiction became heavier and the amount of smoking increased. Therefore, smokers who relapsed after a previous quit attempt were reluctant to make another try.
“When you try to persuade some smokers to quit, they arguethat they feel healthy only if they still want to smoke; otherwise, they feel sick.” (Female, 46) Smokers acknowledged that the lack of pharmacological as well as family support was reasons for their relapse in the past quitting effort.They argued the need for a strong willpower to quit smoking. There were high-risk situations where the smokers attempting to quit could hardly stay abstinent as they felt embarrassed to refuse if others offered you cigarettes.
“I am able to control myself [not to smoke] in public areas, but when I stay alone and think about problems, …., [I cannot resist smoking].” (Current smoker, male, 43)
Suggestions for modifying the SHI
We presented the existing SHI packageand explained how the intervention would be delivered. Participants were invited to make comments or provide suggestions to help revise the SHI to meet the context of their community.Under this theme, we identified two subthemes: a) content of the SHI, b) relating certain diseases to subjects’ health conditions, and c) engagement of the whole family.
Content of the SHI
Participants thought that the overall contents of the SHI was relevant and important.They suggested to update some of the text and use powerful languages in the counseling messages to underline the health hazards of smoking and SHS exposure.
“I think it is good to shock people with strong messages about the adverse effects of smoking…. mention something relevant to adults and to children. For example, saying that smoking will make you ‘sexually inactive (impotent)’….and that your child will be ‘intellectually poor’ if he/she exposes to cigarette smoke regularly ………” (Female, nonsmoker, 37)
In the discussions, participants emphasized that smoking cessation was not easy to accomplish so that instead of just informing the subjects of the harm of smoking, it was vital to offer feasible and effective methods to help them quit.
“It is infeasible to ask them [smokers] to quit at once, …, it seems more possible to quit by gradually reducing the amount of smoking…….or by taking quit smoking medications…..but there is no medication in our community.” (A male who tried smoking when young,35)
To implement household smoking restrictions, participant suggested to convince the smoker by showing some real time data about the health hazards among their children from SHS exposure (e.g. results of children’s urine tests). The participant thought that by seeing a positive cotinine test results, parents and grandparents will more likely to make behavioral changes.
“It is unnecessary to explain health hazards; instead, to tell them directly what to do – for example, they cannot smoke at home or they must take a shower after smoking, …, they learned about the harm of smoking and soon they forgot – it is useless…..By showing them the urine cotinine results of children and the meaning of this will raise concerns among the household smokers about the child’s health… ” (A female whose father smokes, 29) Participants in the FGDs made suggestions for simplifying the language for some of the health risks associated with cigarette smoking and SHS exposure of children.
“What’s this one mean? Increased risk of sudden infant death syndrome, how do you mean? I don’t understand that word.” (Male, Smoker, 45)Another said, “I do not understand ‘chronic obstructive pulmonary disease (COPD)’ is it something that blocks the throat? ….can we replace with ‘disease that will make it difficult for you to breathe normally?” (Female, non-smoker, 39).
Personalizing the advice by relating certain diseases to subjects
Health conditions or other relevant information
Considering some smokers did not believe smoking damages their health, it was essential to point out certain kinds of diseases they have were related to smoking. If the subject was completely healthy, this approach might work by giving examples of someone else that they know.
“When my son’s (4 years old) asthma attack happens, I show my anger to my husband and blame the attack to his smoking………he never argues and try not to smoke at home……., but after few days he would start smoking again at home…., he also took several unsuccessful attempts to quit smoking after realizing the fact that my son’s asthma exacerbation is related to his smoking at home….” (Female, nonsmoker, 32)
Also, for subjects who thought it was impossible for them to quite due to their repeated failures, some participants suggested that it would be important to increase their confidence by referring to examples of people who have successfully quit.
“One of my friend successfully quitted smoking after he had a boy 4/5 years ago; he would walk away when he would see us (few friends) smoking in the same table; I started follow his path when my wife gave birth of our baby daughter 2 years ago….; it was difficult at the beginning and I bought some quit tablet from Shanghai….; Also, I called my friend many times for his advice and it was very helpful”. (Male, ex-smoker, 36)
Engagement of the whole family
Smokers need support and supervision to maintain abstinence and avoid relapsing. Therefore, the intervention should target at both smokers and their family members. One participant (male, 44) mentioned some male smokers would get annoyed at his wife if she kept asking him to quit smoking. However, they would rather listen to their children’s words.
“Family members usually have stronger wills [to have smokers quit], …, there should be some punishments [if smokers break smoke-free regulations] but engaging the child or health of the child in the discussion will have favorable effect…...!” Support from family or friends may also help in the quitting process.
“I tried to quit few times in the past but failed, which may be because no one supported my effort. If a family member or a friend could continuously remind me and give psychological support, I think it would work on me….I am that kind of person who needs continuous push…” (Male, smoker, 28)
One participant suggested to highlight the importance of the immediate benefits of quit smoking to whole family in the discussion, such as saving money (from not buying cigarettes and reduced cost for health problems), setting god example for the child and improving health of all the family members.
“Counselor can say that by not smoking you will save, for example, RMB 10 per day and RMB300 each month. You can use this savings to go to a nice restaurant for food with your family…………….! Other similar example for healthcare costs (if relevant) can also be made.” (Female, nonsmoker, 43)
Delivery format of the SHI
Participants thought the proposed delivery formats of i) initial in-person counseling (30 minutes), ii) telephone counseling at weeks 1 and 2(15minutes each), iii) in-person counseling in week 4 (20minutes), and iv) telephone counseling in week 8 and 16 (5 minutes each)will be acceptable to most of the rural households who have children.
However, some suggested for brief (3-5 minutes) contacts frequently (i.e. in weeks 3, in between weeks 4, in between weeks 8 and weeks 8 and 16). One participant suggested more frequent contact with those who needs more help and want to discuss more.
“Some smokers may not need more contacts if they are motivated to quit…! However, I would prefer to talk with the counselor more often to help me during the difficult time of quitting process. May be giving us the counselor’s telephone number to call (when needed) would be useful”. (Male, Smoker, 42)
However, another disagreed and suggested for less proactive call. He would prefer receiving frequent (3-4 times weekly) WeChat messages instead of a telephone call.
“I am busy with my business in most of the time……so, when a counselor call to discuss, I might not be in a good position to discuss about smoking cessation…. ; it might be better if I could call at my convenience, . …also, the counselor can send the counseling messages via WeChat….”. (Smoker, Male, 40)
About the pamphlets (developed by the China CDC), participants did not have much to add. They thought it is good, but they were not sure if everyone will read the whole pamphlet. They suggested the use of medium size posters or small board (to palce/hang in the living room or within the house) and stickers (to keep in the car or wallet or hand bags) would work as reminders.
Discussion
This qualitative study explored the views of rural Chinese household members for delivering an intervention to reduce children’s exposure to SHS and promoting smoking cessation among household smokers. Participants considered SHI as an acceptable intervention to support tobacco control in the rural Chinese households. Furthermore, they provided suggestions on the content and design of the intervention, which may improve its acceptability and usability. The SHI intervention and accompanying counselors’ guide was refined with incorporating feedback from the focus groups. Changes or additions suggested by participants were implemented if the majority of participants were in agreement with the change, if it was in keeping with the key components of SHI [16] and its theoretical framework (i.e. protection motivation theory) and if it was practical within the target setting.
Participants who smoked raised several challenging issues in relation to their smoking while most nonsmoking participants held negative attitudes towards smoking behavior, in general, and towards smoking around children or at home. The challenges for smoking cessation, discussed by the participants, included low motivation, heavy addiction, and lack of quit smoking support. Adopting household smoking bans were hindered by showing respect for elders and visitors.
Misconceptions regarding smoking behaviors were still prevalent in China [25]; and ineffective measures such as smoking near windows or by fans that intended to remove impacts of SHS were widely adopted. Decisions of smoking households will directly determine young children’s health. Nichter et al. [26] suggested smoking bans in the home could be effectively promoted as an important cultural value linked to male responsibility to protect the health of the family. In practice, mothers of the child were most often credited with initiating a discussion regarding the implementation of a smoke-free policy to address SHS exposure in the home [27]. Hence, instead of targeting only at smokers, smoking hygiene intervention should be tailored to nonsmoking caregivers’ concerns and needs. These nonsmokers could then initiate discussion and support the smokers, who are mostly male, in following smoking restrictions at home/cars and taking steps towards quitting smoking.
In China, especially in rural communities, it is typical for more than two generations living together. Smoking by older household members or visitors was blamed as the main barrier to implement and maintain a smoke-free policy [28], which is consistent with our findings. Young parents faced sociocultural and environmental challenges for establishing smoke-free home rules, mainly due to their high respect for elderly guests [29]. It is deemed as impolite to restrict smoking in the home when elders come; and even nonsmokers will provide guests with cigarettes [30]. To address this problem, the enforcement of smoke-free policies in the workplaces and public places should be promoted,which results in a shift in social norms and ultimately in more voluntary smoke-free homes [31]. Other measures as suggested by the participants in the focus groups could also be useful: engaging children to deliver tobacco control messages to elderly and visitors, posting no-smoking signs or other anti-tobacco messages within the households, and buying quit smoking medications for elderly as gifts.
Previous studies showed that smoke-free homes were associated with increased cessation among smokers and decreased cigarette consumption [32,33]. Therefore, it is inspiring to combine smoking cessation with SHS exposure reduction as the focus of smoking hygiene intervention. Erol and Erdogan [34] claimed behavior changes could occur when perceiving high benefits and low barriers. In our context, the primary motivation for smokers to change smoking behaviors was to reduce the adverse effects of smoking and protect their children from SHS exposure. To strengthen motivators among the smokers, it is important to emphasizethe hazards of tobacco use to themselves and to their loved ones (e.g., spouse, children), and to generate recognition of benefits of quitting.
Participants suggested to clarify some of the counseling messages by delivering direct health impact information and to provide more personalized information (i.e., information that has more personal values to the target subject which would vary from individual to individual). We have incorporated most of these suggestions in the development of our tailored SHI intervention. Participants also suggested to use biochemical measures (i.e., urine cotinine value of the child) to motivate smokers and other household members to engage in the family tobacco control intervention. Previous studies [35,36] also reported the use of biochemical measures as a motivational trigger to promote tobacco exposure reduction and smoking cessation. However, due to the logistical reasons (i.e.delay in collecting urine sample for some subjects, time required to get the results of the urine cotinine test from our laboratory, and the timing of the subsequent follow-up counseling sessions) did not allow us to consider this in the current intervention. It suggested that future studies targeting the same population group consider including feedback of biochemical measures in the design of the intervention delivery.
Strengths and limitations
It was the firstqualitative study targetingthe rural population in China that focused on addressing the issue of SHS exposure among young children as well as quit smoking in adults.The intention of the study was to improve the acceptability and usability of the SHI to rural Chinese households with children. This formative study conducted in our target end users has informed the modification of content and design of the existing SHI intervention. There are few limitations of this study. First, the study setting (i.e. rural Taizhou) that we selected was relatively economically developed compared to the rural areas in Western China. Second, the FGDs faced recruitment bias as the participants were recruited via online self-registration; also no female current smokers participated in the FGD which might be due to the social taboo of female smoking in China. Third, as participants were parents or caregivers of children (aged 5 years old or below), our findings may not be applicable to households without a child or the general smoking population in China.Fourth, the qualitative study was relatively small (N=18), although the study endpoint was determined by data saturation.
Conclusions
This formative qualitative study in rural Chinese household members provides insights about the need and delivery of a smoking hygiene intervention to reduce SHS exposure among children living in smoking households in rural China. The findings informed the modification of an existing intervention model (SHI) and improved the quality of the final intervention to develop a revised model (i.e.SHI-Rural) for use by the rural Chinese household members, which is now being evaluated in an ongoing randomized controlled trial in China.
Author Contributions
ASA and ZP conceived the study. XX and XXC oversaw the overall implementation of the study and provided training to data collectors. HJ and ZP supervised the field data collection. ZP conducted the analyses with guidance from ASA. ZP and XXC worked together to prepare the first draft of the manuscript, which was then distributed to all the co-authors for comments. HJL, HW critically reviewed the first draft of the manuscript and provided useful insights. All authors approved the final draft of the paper.
Disclaimer
The funding body had no role in the design or conduct of the study, collection, management, analysis and interpretation of the data, or preparation, review and approval of the manuscript.
Conflicts of interests
None declared.
Ethics approval
The study was reviewed and approved by the Ethics Committee of Duke Kunshan University (IRB No: 2016ABDU003).
Data sharing statement
The data used and analyzed in this study can be available from the corresponding author on reasonable request.
Acknowledgments
The authors thank the study participants for their participation in this study and the Taizhou CDC to arrange the focus groups. This study was supported by the National Natural Science Foundation of China (NSFC) [Award number: 71673125]. The funders had no role in the design or conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review, and approval of the manuscript.
References
1. Sheahan, SL, FreeTA. Counseling parents to quit smoking. Journal of Pediatric Nursing. 2005; 31(2): 98-102, 105-109.
2. Warren CW, Asma S, Lee J, et al. Global Tobacco Surveillance System: The GTSS Atlas 2009.
3. GillilandFD, Li YF, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. American Journal Respiratory Critical Care Medicine. 2001; 163(2): 429-436.
4. Oberg M, Jaakkola MS, Woodward A, et al. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet. 2011; 377: 139-146.
5. Li Q, Hsia J, YangG. Prevalence of smoking in China in 2010. New England Journal of Medicine. 2011; 364: 2469-70.
6. Li L,ChenQL. Patterns and burden of tobacco use in China. China Health Economics. 2008; 27: 26-30.
7. Liu Y, ChenL. New medical data and leadership on tobacco control in China. Lancet, 2011; 377: 1218-1220.
8. The World Health Organization? Global Adult Tobacco Survey (GATS) China Fact Sheet 2010.
Li C, WangLM, Huang ZJ, et al. Survey of degree of passive smoking exposure and related risk awareness in adults in China. 2013. Zhonghua Liu Xing Bing Xue Za Zhi. 2017; 38(5): 572-576.
9. Yao T, Sung HY, MaoZ, et al. Secondhand smoke exposure at home in rural China. Cancer Causes Control. 2012; 23(1): 109-15.
10. Merom D, RisselC. Factors associated with smoke-free homes in NSW: Results from the 1998 NSW Health Survey. Australian and New Zealand Journal of Public Health. 2001; 25: 339-345.
11. AAP. American Academy of Pediatrics Committee on Substance Abuse. Tobacco’s toll: implications for the pediatrician. Pediatrics. 2001; 107: 794-798.
12. Kegler MC, Escoffery C, Groff A, et al. A qualitative study of how families decide to adopt household smoking restrictions. Family Medicine and Community Health. 2007; 30(4): 328-341.
13. CramerM, RobertsS,XuL. Evaluating community-based programs for eliminating secondhand smoke using evidence-based research for best practices. Family Medicine and Community Health. 2007; 30(2): 129-143.
14. EscofferyC, MullenP, Genkin B, et al. Coaching to create a smoke-free home in a brief secondhand smoke intervention. Health Education Research. 2017; 32(6): 555-568.
15. Abdullah AS, Hua F, Khan H, et al. Secondhand Smoke Exposure Reduction Intervention in Chinese Households of Young Children: A Randomized Controlled Trial. Academic Pediatrics. 2015; 15(6), 588-598.
16. Yan Y, Jacques-TiuraAJ, Chen X, et al. Application of the protection motivation theory in predicting cigarette smoking among adolescents in China. Addictive Behaviors, 2014; 39(1): 181-8.
17. Tang, X, Yang, F., Tang T., et al. Advantages and Challenges of A Village Doctor-Based Cognitive Behavioral Therapy for Late-Life Depression in Rural China: A Qualitative Study. PLoS One, 2015; 10(9): e0137555.
18. Craig P, DieppeP, MacintyreS, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ, 2008; 337: a1655.
19. DamschroderLJ, Aron DC, Keith RE, et al. Fostering Implementation of Health Services Research Findings into Practice: A Consolidated Framework for Advancing Implementation Science. Implement Science, 2009; 4: 50.
20. Rogers RW, A protection motivation theory of fear appeals and attitude change. The journal of Psychology. 1975; 91: 93-114.
21. Taizhou Bureau of Statistics. Statistical Bulletin of 2017 National Economic and Social Development of Taizhou. Retrieved October 26, 2018, from:
22. Xu Y, Wu Q, Xu SY, et al. Current research of passive smoking exposure in Zhejiang. Disease Surveillance. 2012; 27: 887-90,897.
23. XuY, XuS, WuQ, et al. Association between secondhand smoke exposure at home and cigarette gifting and sharing in Zhejiang, China: a repeat cross-sectional study. BMJ Open, 2016; 6(3): e010058.
24. Ma S, Hoang MA, Samet JM, et al. Myths and attitudes that sustain smoking in China. Journal of Health Communication. 2008; 13(7): 654–66.
25. NichterM, PadmajamS, NichterM, et al. Developing a smoke free homes initiative in Kerala, India. BMC Public Health. 2015; 15: 480.
26. Berg CJ, Zheng P,Kegler MC. Perceived benefits of smoke-free homes, the process of establishing them, and enforcement challenges in Shanghai, China: a qualitative study. BMC Public Health, 2015; 15: 89.
27. Zheng P, Berg CJ, Kegler MC, et al. Smoke-free homes and home exposure to secondhand smoke in Shanghai, China. IntJouof Environmental Research and Public Health. 2014; 11(11): 12015-12028.
28. Robinson J, Ritchie D, Amos A, et al. “Waiting until They Got Home”: gender, smoking and tobacco exposure. Social Science & Medicine. 2010; 71: 884-90.
29. Wang CP, Ma SJ, Xu XF, et al. The prevalence of household second-hand smoke exposure and its correlated factors in six counties of china. Tobacco Control. 2009; 18: 121-126.
30. St Claire AW, Boyle RG, Schillo BA, et al. Smokefree home rules adoption by smokers and nonsmokers: Minnesota, 1999-2010. Ame Jour of Preven Med. 2012; 43(5 Suppl 3): S197-S204.
31. Pizacani BA, Martin DP, Stark MJ, et al. A prospective study of household smoking bans and subsequent cessation related behaviour: The role of stage of change. Tobacco Control. 2004; 13: 23–28.
32. Mills AI, Messer K, Gilpin EA, et al. The effect of smoke-free homes on adult smoking behavior: a review. Nicotine and Tobacco Research. 2009; 11(10): 1131-1141.
33. Erol S, ErdoganS. Application of a stage based motivational interviewing approach to adolescent smoking cessation: the Transtheoretical Model-based study. Patient Education and Counseling. 2008; 72: 42–8.
34. Wilson SR. A controlled trial of an environmental tobacco smoke reduction intervention in low-income children with asthma. Chest. 120; 1709–1722 (2001).
35. HutchinsonSG, van BreukelenG, van SchayckCP, et al. Motivational interviewing and urine cotinine feedback to stop passive smoke exposure in children predisposed to asthma: a randomised controlled trial. Sci Rep. 7; 15473 (2017).
Received: November 06, 2020;
Accepted:November 17, 2020;
Published: November 24, 2020.
To cite this article : Pan Z,Chen X,Zheng P, et al.Developing A Community-Based Tobacco Control Intervention to Reduce Secondhand Smoke Exposure Among Children and Promote Smoking Cessation Among Household Members in Rural China: a Qualitative Study. Health Education and Public Health. 2020; 3:6.
©Abu SA, et al.2020.
