Review Article / Open Access
DOI:2020; 3(5): 351- 356 doi: 10.31488 /heph.155
How to Build, Utilize and Deploy the "Disability Registry" to Enhance the PHR System Through out Life in Japan Who Manages Each Person’s Lifelong Outcomes?
Tachibana Tomoko*
Center for Public Health Informatics, National Institute of Public Health.
*Corresponding author: Tomoko Tachibana, MD, MPH, PhD, 2-3-6 Minami, Wako city, Saitama prefecture 351-0197, Japan, Tel: +81-48-458-6206, Fax: +81-48-469-0326
Abstract
In Japan, since 2001, efforts have been started so that all citizens can actively utilize IT and enjoy its benefits to the fullest extent. Then, in the medical field, the PHR (Personal Health Record) service model based on the consent of the person has started to be applied to some diseases. In this study, we verified the application of the PHR model in the construction, utilization, and deployment of the “disability registry” proposed by the authors, to examine its specifics. The “input” and “output” information probably could be covered, by ledger records of local governments and the connection with the existing information. However, the medical certificate and doctor’s opinion at the time of welfare service certification needed to be converted into electronic data that can be analyzed by a software program. Although “outcome” information is an index related to the well-being of life, there was concern about a relative lack of information. Therefore, it is necessary to increase the outcome information by implementing the “Disability App (Figure 2).” Utilization of wearable devices would be useful to reduce the burden of responding to persons with disabilities. In addition, if we prepare a question sentence using ICF classification in the disability application, we can contribute to “promotion from medical model to social model.” If the “disability registry” is constructed and utilized in the PHR model, by managing, inputting, and utilizing information by the individual who is the target of the medical welfare service, it is possible to realize that the subject is the recipient of the service. Not only will the recorded responses of the application be accumulated and analyzed, but the possibility of linking with various government certifications and improving work efficiency will also increase. In order to aim for “construction of a lifelong PHR system for all” in Japan, it will be indispensable to construct and utilize a DB for persons with disabilities using the PHR model. To effectively utilize the ever-increasing social security costs, the construction and utilization of the PHR model “disability registry” is a priority issue for Japan, and it seems that it is necessary to realize it immediately.
Keywords: disability registry, data health, PHR, individual life course, input, output, outcome
Introduction
The COVID-19 pandemic has changed our lives in so many ways. Our day to day living has no doubt been restricted to a smaller social circle, and many of us have turned inward to reflect upon what is most important in our lives. For those of us in healthcare, the context of providing patient care has changed significantly. Telemedicine, specifically using the virtual video visit has become a mode of delivery for patient care that does not require a face-to-face visit. Such telemedicine visits have been accepted via regulation adjustments by the Center for Medicare and Medicaid (CMS) governing telemedicine which have been restrictive for decades. Telemedicine via Virtual Video visits (VVV) is far from new. Telemedicine has been offered to enhance better access to health care for patients and their caregivers living in rural and remote areas highlighting that distance may no longer be a barrier. Within states with large rural populations like Arkansas, telemedicine has been integrated for many years because 73 of 75 counties in the state are designated as medically underserved [3].Even for patients who have access to transportation, the time investment involved in getting to and participating in a health care visit is significant. It involves the time to travel to the health care setting, the waiting room time before being called into the consult or examination room, waiting again for the clinician to come into the room, and then returning home. It has been estimated that this can take a half to a full day even for a visit that may take only 10 minutes with the clinician [4]. Virtual visits have multiple advantages including ensuring patients’ and providers’ safety from viral infection and offer advantages with respect to time- and cost-saving. During COVID-19 pandemic, we are now seeing an exponential growth of VVV.
Promotion of ICT (Information and Communication Technology) Utilization in the Fields of Medical Care, Long-Term Care, and Health
In the past, when a person went to a medical institution due to physical or mental disorders, the medical records and test results at that time were stored as medical records only at the medical institution that performed the medical treatment. Information on prescription drugs and the use of other medical institutions was basically stored in each location. This has been changing in recent years, and efforts are underway to consolidate personal information that has been stored and stored separately in one place. The move is to manage and utilize the information that originally existed as a "paper notebook" by digitizing it and centrally collecting it as data. The accumulated data will be analyzed and utilized by clinical research institutes, etc., and will be useful for the future development of medical care [10] (Figure 1).
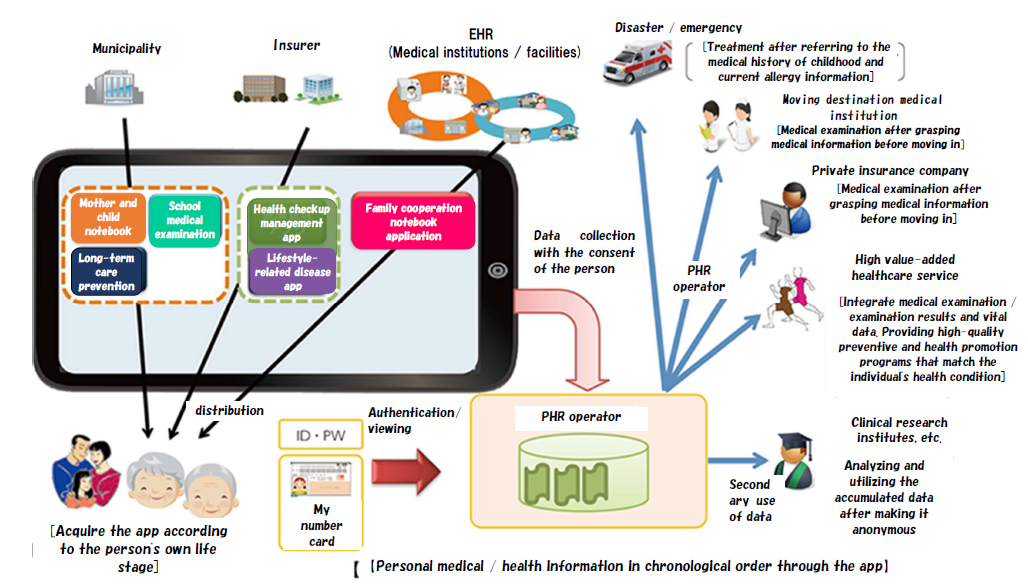
Figure 1. Medical/health/long-term care information model of personal health record. * Borrowed from the Ministry of Internal Affairs and Communications website. The English translation of the figure neutralization is by the author.
What are the Elements that Need to be Added as a "Disability DB"?
Then, what is specifically lacking in the current situation? What do we need to consider in the future? Below, we would like to propose a concrete image of the necessary "disability DB" while grasping the necessary information from each viewpoint of "input," "output," and "outcome" [11] in epidemiology and adding consideration.
Input Information
Input originally means "information input" that captures data into a computer and refers to leaving it as a person's memory or experience. In this case, it is mainly a series of intervention information such as actions related to medical care, long-term care, medical examinations, etc. Currently, the main databases (DBs) that have become apparent and are being discussed are health DBs, medical DBs, and long-term care DBs, and there is a need for a concrete image of the "disability DB" that remains institutionally. The health DB is a database of "specific medical examinations and specific health guidance" provided mainly for the prevention of lifestyle-related diseases such as diabetes and cancer. Utilization of IoT (Internet of Things) devices and GIS (Geographic Information System) [12] is being developed. The medical DB is further composed of various DBs. In addition to NDB [13], NCD [14], cancer registration DB [15], etc., various databases have been constructed as DBs for each disease in academic societies and for each medical institution. The long-term care DB stores about 1.1 billion long-term care receipt information and about 60 million long-term care certification information (as of the end of 2018). Regarding these big data in the medical and long-term care fields owned by the government, provisions for data provision to researchers, etc., and regulations regarding data connection analysis are being developed [16]. To promote the utilization by a wide range of actors, this is while giving consideration to ensuring safety, and to lead to the development of academic research and development. The stored data in the long-term care database is based on the national long-term care health system [17] and is also applied to patients with designated intractable diseases who are over 40 years old. On the other hand, the construction of a database for patients with designated intractable diseases and a database for children with chronic specific illnesses has been promoted [18]. It is thought that there are not a few residents in the younger age group who are difficult to be included in the long-term care health system, such as chronic patients with long-term care and persons with disabilities of various types.
Now, let's think about what input information is necessary for residents who are considered to be "disabled" as a disability database(Figure 2). First, regarding input information related to "medical care," "medical examination," "long-term care," etc., even if a person has a disability, the necessary individual data can be accessed by linking each DB. However, it may be necessary to take care so that access problems such as difficulty in receiving medical examinations do not occur depending on the presence or absence of disabilities. On the other hand, regarding input information related to disability health and welfare services, there is information on "certification" for persons with disabilities and "receipt of disability welfare services" in Japan [19]. It is obligatory for each local government to keep a ledger, and with the national data conversion policy, the movement to consolidate them by electronic data conversion is about to proceed. However, they say, for example, the doctor's written opinion required for "certification" is likely to be stored for each individual with a disability as PDF image information.Though the "doctor's written opinion" is different from the medical certificate, it has the same meanings as the doctor's medical information provision. In other words, the doctor's written opinion describes the objective living functions necessary for judging the "disability support category[20]."If they convert it to image PDF data, they might have been just creating an "electronic version of the ledger." If a "database" is created instead of a ledger of input information, it should be digitized as variable data that can be analyzed quantitatively and qualitatively.

Figure 2. Proposal of PHR service model based on the consent of the person.
Output Information
An output is a computer's "output" to an input. In the medical database, response result data for diagnosis and treatment correspond to this. In addition, the stored output information of the medical examination DB corresponds to the result information of various tests and medical examinations. In the case of the long-term care DB, the direct effect of the various long-term care services provided will be the output. The output information in these "medical DB", "health DB," and "long-term care DB" would exist considered to be recorded and exist in a form that is roughly paired with each input information.
Then, what is the output in the disability DB [Figure 2]? In Japan's welfare plan for persons with disabilities and welfare plans for children with disabilities, outcome goals and activity indicators are set [21]. The "activity index" in this can be regarded as output information in the implementation and evaluation of each policy. Based on the national plan, each prefecture will formulate a plan unique to the local government and improve the measures while repeating the PDCA (Plan-Do-Check-Action) cycle. In other words, the overall picture of the "activity index" of the disability welfare policy promoted by the government is published on the Web. Each local government such as prefectures refers to this and uses it as an evaluation index for measures. It can be expected that the results of service provision / evaluation for each target "individual," that is, the output information, is generally owned by local governments such as municipalities. In addition, it is necessary to digitize these as variable data that can be analyzed quantitatively and qualitatively, and to construct a "disability DB" together with the output information held in units such as public facilities. Furthermore, if you aim to collect detailed output information, you should consider a method in which the individual who receives the service inputs the information. The spread of cloud and mobile devices in recent years has made it possible for oneself to manage and utilize scattered health data. For example, if you use a wearable device such as Fitbit [22] or Apple Watch [23], you can automatically and continuously record data such as heart rate, body temperature, and blood pressure.That's because the Apple Watch has all kinds of sensors, including GPS, barometric altimeters, accelerometers, and heart rate sensors. In addition, if ICF (International Classification of Functioning, Disability) [24]related matters are prepared so that they can be continuously input using ICT, it may be possible to track daily "living functions" in more detail than before.Utilization of wearable devices will be useful for reducing the burden of answering. At that time, if the person himself/herself is willing to answer but cannot perform the input work due to various obstacles, he/she may be able to do so with the support of the surrounding social capital.
Outcome Information
While the above-mentioned output is "output result," the outcome means "result/effect. "The "outcome goals" in Japan's disability welfare plan [25] may be positioned as outcome information in the implementation and evaluation of each policy. So what are the "outcomes" in the disability DB?By the way, the outcome goals of the policies presented by the government are the following five:(1)Transition of facility residents to community life,(2) Construction of a comprehensive community care system for mental disorders,(3) Development of community life support bases, etc. with an eye on the increasing severity and aging of persons with disabilities and "after the death of their parents," (4)Transition from welfare facilities to general employment,etc.,(5)Establishing a system to support children with disabilities.Then, what are the outcomes that should be entered in the "personal life course" called the disability DB?Many of them seem to be related to "the happiness of life."If it is an input item that you have the opportunity to input frequently, it might be something like "ease of daily life," "comfort of the day," "rewarding of everyday life," etc.As the authors have already mentioned, in recent years, the concept of disability has expanded and the concept of health itself has changed along with changes in social conditions such as the medical economy [26].Disability is by no means a "health event to avoid," as it used to be.People face various challenges, physically, mentally and socially, in the course of their lives.Therefore, as a result, they may spend their lives afterwards with various "sequelae, disabilities, and chronic injuries/diseases." The fact that "what you can't do" increases will be also common to "aging." Even if someone is "a person with vulnerability" who has such disabilities, he/she can control his/her own life to make his/her life as comfortable as possible. From here on, "disability" would like to be used in this paper as "vulnerable health" as we had suggested.In other words, please note that from here, "disability" in this paper is regarded as "people who live with physical, mental, and social challenges related to health."
Values vary from person to person.Therefore, of course, the outcomes of each aim will vary from person to person.ICT may be useful for inputting information in such cases(Figure 2).In other words, as mentioned in the output in the previous section, if you use the cloud and mobile devices that have become widespread in recent years, you can expect to continuously collect detailed personal outcome information.In addition, by developing and utilizing the iPhone [26] application, it is possible to collect more efficient and high-quality outcome information.For example, on the smartphone drawn on the right end of [Figure 2], develop a dedicated "disability app" with questionnaire items.In case, if you download it in advance, how about allowing individuals who are recipients of disability welfare services to enter the required outcome information?Outcomes would be indicators of life's well-being and comfort. If so, how accurately can a third party grasp the outcomes for each individual? In order to enhance the outcome information, it will be important for "the person him/herself" to enter it. However, for people living with disabilities, sometimes it may not be possible for them to enter information on their own.At that time, if the individual is willing to answer but cannot enter each response, the problem might be solved if he/she agrees to cooperate with the social capital [28], that is, human relationships such as trust and relationships, local community organizations and volunteer organizations, etc., around him/her.
Considerations
We examined the concept of "disability DB" with the residents who are difficult to be covered by the long-term care insurance system, etc., while living their daily lives with intractable diseases and chronic injuries including disabilities.In order to develop the construction and utilization of the disability DB, it seemed to be important to organize each "input," "output," and "outcome," and to make the best usage of ICT, according to the individual life course.Regarding Apple Watch, on September 4, 2020, the added electrocardiogram function was approved as a medical device in Japan as well.In the future, for example, these devices may be able to be used for solving challenges such as:“How does biometric sensor data obtained from continuous monitoring of oxygen saturation and blood glucose relate to measured values and rate of change in temperature, humidity, and barometric pressure, and what kind of fluctuations will occur in individuals with disabilities?”By conducting such research, there is a great need to explore the relationship between changes in physical condition and climate change in people with disabilities.By clarifying them, the benefits for Japan, which has many natural disasters, will never be small.For example, when a typhoon approaches, it leads to consideration of "what should be prepared at the evacuation center of the local government."
As described above, there were a lot of great merits in utilizing the information support environment that has advanced due to the spread of the cloud, mobile devices, and wearable devices in recent years as an element of the disability DB.In Japan, the Ministry of Health, Labor and Welfare established a project team in the field of maternal and child health in January 2018 under the "Data Health Reform Promotion Headquarters [29]." This rational flow of data integration could be said to be the movement in the field of "maternal and child health" throughout infancy and school age, following the utilization of health information related to lifestyle-related diseases such as diabetes and cancer. At the study group, "minimum information to be digitized" and "selection of medical examination items that will be the standard electronic recording format," about infant medical examinations (3-month-old child, 18-month-old child, 3-year-old child) and pregnant women medical examination information, were promoted [30,31]. The steps for integrating and utilizing distributed data can be considered to be basically the same process as for lifestyle-related diseases such as cancer.
So how should we manage that integrated information? Japan has a social security/tax number system, that is, "My Number System [32]." Each Japanese is given a designated 12-digit number as his/her own My Number. Therefore, a legal system should be put in place so that this can be used as a personal identification number. Currently, distributed data of health care, welfare, and long-term care is the personal information of the people [33], so the "use" such as the provision and scope should be uniquely decided by the people/patients/parties concerned. The My Number Card is scheduled to be used as an insurance card in 2021 by the Ministry of Health, Labor and Welfare [34]. If My Number is used as an individual identifier in the "disability DB" and will be linked with medical information, “support needs owners” who live with sequelae and acquired disabilities can be reassessed as prognosis/outcomes for various injured patients. By doing so, it is possible to contribute to the quality improvement of the intervention of local health care and welfare services for various persons who cannot receive adequate care.In addition, it will also be possible to enhance the database information, such as linking output/outcome information for medical interventions related to many injuries and illnesses [26]. When the identifier is an individual in the construction of DB, it is informologically PHR [35]. PHR is a mechanism for patients to collect and centrally store their own medical and health information. It is said that the quality of medical care and the efficiency of operations can be improved by utilizing information by providing it to medical institutions. Many reports have already been made on research using PHR, including in the United States [36,37]. The advantage of PHR using My Number is considered to be great in that it is possible to clarify the responsibility for human rights and information ownership and to clearly indicate that the owner of personal information is the "person of the patient/parties concerned, etc."
Finally, we would like to describe the process and points of the future construction and utilization of the disability registry DB, along with its significance. As mentioned above, the concept of "disability" has changed from "disability in a narrow sense" of "physical disability, intellectual disability, and mental disorder" to "some kind of health vulnerability such as injury or illness." However, the data on "disability" so far is expected to be extremely small except when it is caused by "aging" or "intractable disease" or when it is closely related to medical care. This seems to be because the "disability" health and welfare field has been classified into the humanities field rather than the natural sciences. Therefore, “input” and “output” information aside, it will be necessary to add and enhance “outcome” information. So how do we increase the outcome information? As already mentioned in this study, outcome information is a matter of "inherent life happiness to be achieved." Therefore, it is important to allow "the person/patient/party" to input the intention. At that time, it will be helpful to use a device such as a smart watch that we can "wear" and "continuously measure and record" biological data. Furthermore, in the case of maternal and child health mentioned above, a "mother and child notebook application" was installed on the smartphone. Similarly, how about developing and making/setting up a "disability application including disability notebook (tentative name)" for individuals to manage and record data? If you devise a smartphone disability app (tentative name) so that you will want to access it many times in a fun way, even when you "enter outcome information" into the app, the task will not be a big deal. Combined with information that he/she wants to see repeatedly every day, or that he/she needs to check every day, he/she might be able to get consent and answers to a simple survey. At that time, it is necessary for the question text to ask about "living function," "background factor," etc. according to the ICF classification. This is inorder to let shift to a "social model" instead of a "medical model" when constructing a disability database. Furthermore, if it is possible to associate the disability application with the registration/information providing site related to "disaster assistance information," the service provider such as firefighting/emergency medical services will not have to take charge of everything. From the perspective of disaster health crisis management, if the community wants to prepare for "disabled people" who have some kind of vulnerability in normal times, not only the specialized occupations of health care, welfare, and long-term care, but also police, fire departments, and patient family associations, etc. It is necessary to systematically and widely carry out a wide range of cross-cutting cooperation such as family associations and self-government associations at the national, prefectural, municipal, and private levels. Even in such cases, it was thought that the expertise of social medicine should be utilized.
Conclusion
The construction and utilization of the "disability registry" in the PHR model had the following advantages and precautions. In order to more efficiently and effectively utilize the ever-increasing social security costs, the construction and utilization of the PHR model "disability registry" seems to be an urgent priority to be realized in Japan.
We can expect the enhancement of outcome information utilizing ICT.
Clearly indicate that "the patient/party is the main subject."
Efficient and effective services can be expected by accumulating and analyzing input/output/outcome information.
Combined with questions according to the ICF classification, it can contribute to the realization of the flow of "from medical model to social model."
Combining the input information with various administrative certification operations could contribute to the efficiency of operations.
Wearable devices can be worn to reduce the burden on respondents.
Information consolidation can scientifically reduce disparities and interruptions between disciplines and contribute to the construction of a scientific, lifelong PHR system for all.
When converting medical certificates and doctors' opinions when welfare services are certified into electronic data, it is necessary to convert them into data that can be analyzed in the natural sciences.
It is necessary to widely convey that "disability" is "people who live with physical, mental and social challenges related to health."
References
1.Tachibana T. Research on measures for chronic injury and illness in a mature society.In addition to reports on efforts for self-management support research for patients and their families after chronic injury and illness.33rd Public Health Information Research Council Study Group; Jan 2020;Saitama:40.
2.Miyata H, et al. Japan's vision for health care in 2035. Lancet. 2015;385(9987):2549-50. doi: 10.1016/S0140-6736(15)61135-7.
3. The World Bank. Universal Health Coverage for Inclusive and Sustainable Development.
4. Ministry of Foreign Affairs of Japan. JAPAN SDGs Action Platform.
5.Cabinet Office. Society 5.0.
6. Ministry of Health, Labour and Welfare. Meeting of experts on analysis infrastructure for medical / long-term care data, etc.
7. Ministry of Health, Labour and Welfare. Study group on promotion of PHR for public health promotion.
8. Tachibana T, et al.Policy review on building a “Disability Registry” as a prognosis / outcome indicator.Aiming to realize the definition of health for the Care-focused Mature Society.Nerotraumatol.2018;41(1):1-15.
9. Tachibana T. How to support Self-Management for Chronic Injuries/Diseases Based On EBM: Evidence-Based Med. 2020; 3(5): 339-342.
10. Ministry of Internal Affairs and Communications, Japan. Information and Communications in Japan. WHITE PAPER2018.
11.Centers for Disease Control and Prevention. Principles of Epidemiology in Public Health Practice, Third Edition. An Introduction to Applied Epidemiology and Biostatistics.
12. Geospatial Information Authority of Japan. What is GIS.
13. Ministry of Health, Labour and Welfare. Japan. NDB open data.
14. Western Pacific Region of World Health Organization. Preliminary Meeting for the Technical Advisory Group for Noncommunicable Disease Prevention and Control in the Western Pacific Region, Virtual Meeting, 1-30 June 2020: meeting report.
15. National Cancer Center Japan. Cancer registration / statistics.
16. Ministry of Health, Labour and Welfare. Promotion of scientific long-term care, further utilization of long-term care-related DB, etc.
17. Ministry of Health, Labour and Welfare. Outline of long-term care insurance system.
18. Ministry of Health, Labour and Welfare. Homepage about designated intractable disease patient database and pediatric chronic specific disease child database.
19. Ministry of Health, Labour and Welfare. Service usage procedure. )
20. Ministry of Health, Labour and Welfare. Disability support classification.
21. Ministry of Health, Labour and Welfare. Achievement goals and activity indicators.
22. Jo A, et al. Is There a Benefit to Patients Using Wearable Devices Such as Fitbit or Health Apps on Mobiles? A Systematic Review. Am J Med. 2019;132(12):1394-1400.e1. doi: 10.1016/j.amjmed.2019.06.018.
23. Raja JM, et al. Apple Watch, Wearables, and Heart Rhythm: where do we stand? Ann Transl Med. 2019 Sep;7(17):417. doi: 10.21037/atm.2019.06.79.
24.World Health Organization. International Classification of Functioning, Disability and Health (ICF). Classifications.
25. https://web.archive.org/web/20181018004751/http://www.who.int/classifications/icf/en/
26. Ministry of Health, Labour and Welfare. Achievement goals and activity indicators.
27. Tachibana T. Commentary to “the Review for Promoting Evidence-based Healthcare and Welfare Policies for People with Disabilities”: Why is the “Definition of Health for a Care-focused Mature Society” we proposed needed in Japan?" Health Educ and Public Health. 2019; 2(1): 142-4.
28. Harrison AM, Goozee R. Psych-related iPhone apps. J Ment Health. 2014;23(1):48-50. doi: 10.3109/09638237.2013.869575.
29. Coleman J. Foundations of Social Theory (Belknap Press). Published by Belknap Press. ISBN 10: 0674312252ISBN 13: 9780674312258.
30. Ministry of Health, Labour and Welfare. Data Health Reform Promotion Headquarters.
31.Yamagata Z. Utilization of maternal and child health information in the age of data health.
32. Ministry of Health, Labour and Welfare. Promotion of data health in the field of maternal and child health.
33. Cabinet Office. Outline of Duties, Cabinet Office, Government of Japan.
34. Linguee.Personal Information Protection Law (2003).
35. Cabinet Office. My number card (social security, tax number system).
36. Fields RW, Gandhi N. Tools for Population Health Management. Prim Care. 2019;46(4):529-538. doi: 10.1016/j.pop.2019.07.012.
37. Ball MJ, Costin MY, Lehmann C. The personal health record: consumers banking on their health. Stud Health Technol Inform. 2008;134: 35-46.
38. Sidhaye VK, Nishida K, Martinez FJ. Precision medicine in COPD: where are we and where do we need to go? Eur Respir Rev. 2018;27(149):180022. doi: 10.1183/16000617.0022-2018.
Received: October 16, 2020;
Accepted: November 02, 2020;
Published: November 04, 2020.
To cite this article : Tomoko T.How to Build, Utilize and Deploy the "Disability Registry" to Enhance the PHR System Through out Life in Japan Who Manages Each Person’s Lifelong Outcomes?Health Education and Public Health. 2020; 3:5.
© Tomoko T.2020..
