Research Article / Open Access
DOI: 10.31488/HEPH.180
Impact of Nutrition Education Videos on Child Feeding Practices in Urban Informal Settlements of Nairobi
Patricia Jebet Kiprono*1, Judith Kimiywe2, Sharon Iron-Segev1
1. Robert H. Smith Faculty of Agriculture, Food and Environment, Institute of Biochemistry, Food Science, and Nutrition, School of Nutritional Sciences, Hebrew University of Jerusalem and The International School of Agricultural Sciences, Rehovot, Israel
2. Kenyatta University, Kenya
*Corresponding author:Patricia Jebet Kiprono, Robert H. Smith Faculty of Agriculture. Food and Environment, Institute of Biochemistry, Food Science, and Nutrition, School of Nutritional Sciences, Hebrew University of Jerusalem, Rehovot 76100, Israel, Tel: +254726391515
Abstract
Objective: To assess effectiveness of using nutrition education videos to improve knowledge, attitudes and practices to improve feeding practices among mothers in urban informal settlements in Nairobi. Design: A post-intervention study design with intervention and control groups. Setting: Medical-centers in Nairobi’s urban informal settlements. Participants: Caregivers with children 0-23 months in the intervention (n=122) and control (n=120) medical centers in urban informal settlements of Nairobi. Participants in the control arm received standard government care (health talks and counselling) while those in the intervention arm received standard government care plus nutrition education videos, a form of behavior change communication. The intervention was based on a conceptual framework; the Social Behavior Change Communication (SBCC) Pathways to Improved Maternal Infant and Young Child Nutrition Practices and Status. Results: Exclusive Breastfeeding (EBF) was higher in the control arm (92.5% vs 55% (P<0.001). Minimum Acceptable Diet tended to be higher in the intervention arm (38% v 29%). No significant differences in most knowledge and attitude scores were observed. The association test showed that mothers who expressed difficulty in practicing EBF were likely not to practice EBF (P=0.006). The multivariate analysis showed that the odds of participants in the intervention to practice EBF was 0.9 times less compared to the controls (OR 0.90 [95% CI: 0.02 – 0.51] with P=0.006). Conclusions: Increase in knowledge does not always translate to adoption of practices. A combination of nutrition education strategies; facility-based, home-based and peer support should be considered to encourage adoption of practices and increase contact with health workers and peers.
Keywords: Exclusive breastfeeding, complementary feeding, nutrition education videos, interventions, kenya, urban informal settlements
Introduction
The World Health Organization (WHO) recommends initiation of breastfeeding within the first hour of birth, breastfeeding on demand and exclusive breastfeeding (EBF) for the first 6 months of life. This should be followed by the introduction of safe and adequate complementary foods with breastfeeding continuing up to 2 years and beyond allowing for optimal growth and development [1]. Poor feeding practices, as one of the underlying causes of undernutrition, may have short term consequences including morbidity, or long term consequences such as impaired cognitive development and growth deficits [2].
The rates of undernutrition have decreased globally but the numbers are still high in Africa and Asia. In Africa, stunting levels are at 30.3% and wasting at 7.1% while Eastern African countries report stunting prevalence of 35.6% and wasting at 6.0% [3]. Undernutrition in Kenya has decreased over time with current stunting levels at 26%, with 4% wasting and 11% underweight among children less than 5 years of age. Overall, breastfeeding and complementary feeding practices in Kenya have improved but recommendations have not been fully achieved. It was reported that only 61% of children under the age of 6 months were exclusively breastfed and 81% of children received complementary foods at the recommended age with continued breastfeeding. However, only 22% of the children were fed according to the three recommended Infant and Young Child Feeding (IYCF) practices, which are: achieving minimum dietary diversity, minimum meal frequency and minimum acceptable diet [4].
In Nairobi urban informal settlements, a Global Acute Malnutrition (GAM) prevalence rate of 4.6% was reported with 11.4% prevalence of underweight and 26.1% stunting (7.7% severely stunted) [5]. Sub-optimal breastfeeding and complementary feeding practices have been observed in the urban informal settlements of Nairobi due to the unique challenges that these populations face such as food insecurity, poverty, poor sanitation and inadequate hygiene practices. EBF rates in Kibera urban informal settlements, which is located close to the Nairobi Central Business District and has a population of 985.70 inhabitants/hectare was 2%, while Korogocho with a population size of 588.93 inhabitants/hectare had 15% EBF rate [5-7].
Food insecurity has been reported to be a challenge in many informal urban settlements in the world including Kenya [8-10] which could be a contributing factor to high malnutrition rates that reach up to 40% among children under the age of 5 years in these areas [6]. A study conducted in western Kenya, documented an association between low breastmilk intake and household food insecurity [11]. Maternal knowledge as shown in a Kenyan study is another factor that influences child feeding practices and consequently their nutritional status [12]. There is dire need for interventions that will improve feeding practices for children in Kenyan urban informal settlements.
Nutrition education interventions have been implemented. The aims include improving mothers’ knowledge and modifying practices. Exclusive breastfeeding and proper complementary feeding practices can improve the nutritional status of young children [13-15]. The Baby Friendly Hospital Initiative which was launched by the WHO and UNICEF has led to improved breastfeeding practices in Kenya [16]. A nutrition education study conducted in Turkana, Kenya targeting mothers and their spouses showed improvement in the quality of complementary foods given to children under 5 years of age [17]. Similarly, other studies have shown the effectiveness of nutrition education and male partners involvement [18-21].
Nutrition education videos have also been used as an intervention to improve Maternal Infant and Young Child Nutrition (MIYCN) practices [23-26]. A study conducted in Bangladesh used interpersonal counselling and community mobilizations where videos on nutrition during pregnancy and breastfeeding were presented to all groups in the community. Additionally, discussions on topical issues aimed at promoting an optimal nutritional status were carried out in forums for the husbands. The results showed an improvement on the dietary diversity of the women and their health status [22,23]. In rural India, videos were watched and discussed in small groups aimed at improving MIYCN practices. The videos were very popular and results showed improved knowledge on the various topics presented in the videos [24]. After a conflict in Rakhine state of Myanmar, Save the Children, implemented a project on promoting proper IYCF practices [25]. One of their recommendations was the use of nutrition educational videos to complement mother-to-mother peer support groups. None of the studies showed use of videos in a hospital setting. In Kenyan hospitals, nutrition education and counselling are conducted during the clinic visits with facilitation from the health workers. Some of the education materials used are counselling charts and cards with pictures adopted from UNICEF but not use of videos [26].
Therefore, this study aimed to evaluate if health talks and counselling supplemented with educational videos presenting recommended knowledge, attitudes and practices (KAP) to improve feeding practices among mothers would produce better results when compared to methods currently in place. It was hypothesized that caregivers from the intervention group would have higher rates of exclusive breastfeeding and a larger number would achieve minimum complementary feeding practices than controls. In addition, significantly greater knowledge and healthier attitudes towards infant and young child nutrition would be attained following the intervention.
Methods
Research Design
This post-intervention study was part of a larger study in Nairobi County [27]. The study included mother and child pairs (children < 24 months) attending the Maternal and Child Health (MCH) clinics in health facilities within the urban informal settlements of Mathare North for the intervention and Kahawa West for the control.
The intervention consisted of nutrition education videos and standard care. Nutrition education videos from Global Issues in Local Context (GloCal) based on WHO guidelines were shown on screens during clinic visits that included topics on breastfeeding, complementary feeding and water sanitation and hygiene practices. The intervention clinic (Mathare North) was divided into two main sections: for pregnant mothers and those with children. Mothers with children 0-6 months sat on one side and mothers with children >6 months on the other side. At all visits, anthropometric measurements were taken and recorded in the maternal-child booklet to enable monitoring of growth by nutritionists.
Figure 1 shows the conceptual framework that was adopted in the study indicating the social behavior change communication pathways for improved MIYCN practices. The delivery strategy adopted in this intervention was behavior change communication [28], specifically use of videos for nutrition education.
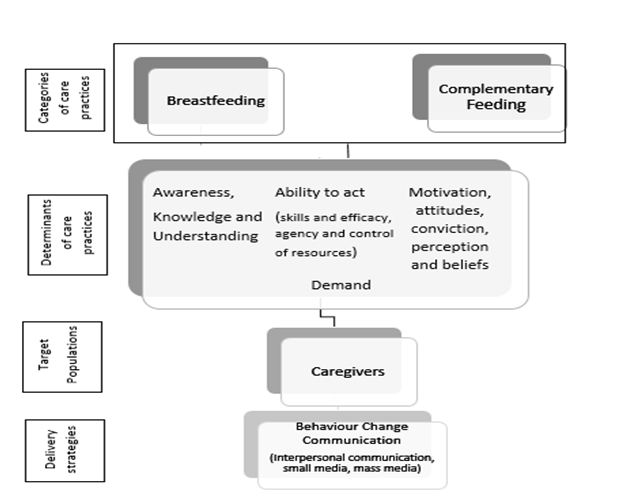
Figure 1:Adapted Conceptual framework of the pathways from Social Behavior Change Communication (SBCC) Delivery strategies to improved Maternal Infant and Young Child Nutrition (MIYCN) practices. Adapted from: SPRING 2014 [24].
Videos were shown on two TV screens for 3 months before an evaluation was done on KAP of mothers. Health workers played 1-2 videos (2-3 minutes on average) as the mothers waited for their appointment after which they paused the videos so they could have further discussions of the videos with the mothers. The videos addressed all age categories and were not tailored for a specific age group. During this methodical break when videos were not playing, health workers allowed discussions and dialogue where mothers could ask questions based on the videos or any other questions. These discussions confirmed whether the mothers understood the message and could hopefully be able to practice with confidence. Clinic staff continued playing more videos throughout the clinic hours. The videos were designed to be colorful and attractive with either real people in real homes and environments or animations that mothers found of interest. Pictures were also used, for example foods and creative visuals where encouraged practices were checked () and discouraged practices marked with an “X”. These videos were designed to be culturally sensitive and foods shown in complementary feeding videos were locally available foods. The videos were in Swahili, thus understood by the targeted audience. The audio used was at an appropriate pace and was clear with written captions at the bottom of the screen. As seen in Table 2, 120/121 (99.17%) had attained some form of education from primary-tertiary, thus a high literacy rate. The video sessions (showing videos then discussing with the mothers) and health talks lasted about 20-30 minutes every day.
The control group were not shown videos. However, they received standard care of health talks provided by nutritionists and/or health workers in the clinic on nutrition and health education to mothers attending the well-baby clinic. The health talks were conducted on a daily basis.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Kenyatta University Ethics Committee. The study was approved by Kenyatta University Ethical Review Board/Committee, KU/ERC/APPROVAL/VOL.1 (217). Written informed consent was obtained from all participants.
Participants
The sample size was a total of 242 mother and child pairs from both clinics determined using the formula of Yamane [29]. Clinic records were used to identify eligible participants. Eligibility criteria included mothers who went to either of the two clinics, had healthy children aged 0-23 months, and consented to be part of the study. For the intervention group, only women who confirmed that they had watched the videos were included. Stratified sampling was used where the mother and child pairs were divided into categories by age according to the WHO [30]. The distribution of children across age categories was done purposively as follows: 0-5 months: 80 (40 from each group), 6-11 months: 82 (42-intervention, 40-control), 12-17 months: 40 (20 from each group), 18-23 months: 40 (20 from each group). The larger numbers in the first two categories were deliberate as it was critical to capture breastfeeding practices between 0-5 months of age and transition to complementary feeding, 6-11 months. A consecutive sampling procedure was used to recruit participants to the study until the sample size was reached.
Data collection
In this study, a semi-structured, researcher administered questionnaire adapted from the WHO [31] was used to collect data among study participants. The questionnaire had sections on socio-demographic characteristics (age, education, number of children), knowledge questions (with two to multiple answers that were pre-analyzed as ‘knows’ or ‘don’t know’, attitude questions [determined whether one had a positive, negative or neutral (neither very good nor very bad) attitude towards a certain practice] and practices regarding MIYCN. This questionnaire had been previously tested for validity and reliability and had been used in Kenyan populations [12,32]. Written questions were used accompanied by picture descriptions to increase comprehension and attitude questions used a three-point Likert scale. The research team underwent training on data collection using the questionnaire. The training included practical use of the questionnaire in pairs and this was followed by discussions on improving the questionnaire. Other minor adjustments or clarifications were done after the first day of data collection. The questionnaire was administered to participants by research assistants through interviews in private spaces at the facilities. After the interview process, the research assistants had reflective and feedback sessions to assess any discrepancies in the collected data. Filled questionnaires were collected by the researcher for data entry and stored safely.
Statistical analysis
Data were coded in MS Excel and then imported to STATA version 15 (STATA Version 15, Stata.Corp., LLC, College Station, TX, 2019) and R statistical software (R Core Team, Vienna, Austria, 2013) for data cleaning and analysis. The key outcomes of interest were exclusive breastfeeding (0-6 months) and minimum acceptable diet (MAD) (6-23 months). MAD was derived from the Minimum Meal Frequency (MMF) and Minimum Dietary Diversity Score (MDD). These scores are validated methods by the FAO (33). MDD is the consumption of 4 or more food groups from the 7 food groups while MMF is dependent on the age of the child and whether the child is being breastfed or not. For example, non-breastfed children of the age of 6-23 months need a minimum of 4 times feeding. MAD is therefore achieved when a child has met both MDD and MMF [30]. To test for significant differences and association between groups, Student’s independent t-test was used on continuous data and Chi-Square or Fisher’s exact test for categorical data where appropriate. P-values of less than 0.05 were considered significant. Univariate and multivariate logistic regressions were used to determine factors affecting outcomes of interest. Table 1 shows the specific indicators used and their interpretation [34].
Table 1.Infant feeding indicators and their interpretation based on WHO recommendations
| Infant feeding indicator | Interpretation |
|---|---|
| Exclusive breastfeeding | Proportion of infants that received breastmilk (including expressed milk or from a wet nurse) without anything else except for Oral Rehydration Salts (ORS), drops and syrups (vitamins, minerals medicines). |
| Minimum Dietary Diversity (MDD) Score | Proportion of children aged 6-23months who consumed food from ≥4 food groups |
| Minimum Meal Frequency (MMF) | Proportion of children (both breastfed and not breastfed) who ate food the minimum number of times. Minimum is defined as:
Breastfed infants 6-8 months: 2 times, Breastfed infants 9-23 months: 3 times, Non-breastfed infants 6-23 months: 4 times |
| Minimum Acceptable Diet (MAD) | Proportion of children aged 6-23 months who attained both MDD and MMF. |
Table 2.Socio-demographic characteristics of participants in an intervention study in Nairobi urban informal settlements (n=242)
| Characteristics | Interventions | ||||||
|---|---|---|---|---|---|---|---|
| Overall N = 242 | SD | Videos + Nutrition counselling N = 122 | SD | Nutrition counselling only N = 120 | SD | P-value | |
| Caregiver’s characteristics | |||||||
| Mean age in years (SD) | 26.93 | 5.99 | 27.19 | 5.52 | 26.68 | 6.45 | 0.51 |
| Mean number of children (SD) | 2.00 | 1.06 | 2.06 | 1.11 | 1.95 | 0.99 | 0.40 |
| Education, n (%) | 0.69 | ||||||
| None | 2 | 0.83 | 1 | 0.82 | 1 | 0.83 | |
| Primary | 72 | 29.75 | 39 | 31.97 | 33 | 27.50 | |
| Secondary | 120 | 49.59 | 61 | 50.00 | 59 | 49.17 | |
| Tertiary | 47 | 19.42 | 20 | 16.39 | 27 | 22.50 | |
| Child’s characteristics | |||||||
| Female, n (%) | 113 | 46.69 | 55 | 45.08 | 58 | 48.33 | 0.61 |
| Mean age in months (SD) | 9.64 | 5.69 | 9.84 | 5.53 | 9.44 | 5.86 | 0.59 |
| Age categories, n (%) | |||||||
| 0 – 5 months | 80 | 33.06 | 40 | 32.79 | 40 | 33.33 | |
| 6 – 11 months | 80 | 33.06 | 40 | 32.79 | 40 | 33.33 | |
| 12 – 17 months | 42 | 17.36 | 21 | 17.21 | 21 | 17.50 | |
| 18 – 23 months | 40 | 16.53 | 21 | 17.21 | 19 | 15.83 |
N: Total sample size, SD: Standard deviation, n: numbers in each category. Independent t-tests, chi square and Fisher’s exact where applicable, (*P <.05)
Results
Table 2 describes the socio-demographic characteristics of the study sample.
Exclusive Breastfeeding, Knowledge and Attitudes (0-6 Months)
All children of 0-6 months in both groups were being breastfed. EBF was higher in the control group (92.5%), compared to the intervention group (55%) (P< .001). Despite EBF being lower in the intervention group, half of the participants (50%) had heard of the term exclusive breastfeeding compared to the control where only 20% were familiar with the term (P=0.01). A higher number of mothers in the intervention group, 34 (85%) knew that one had to seek healthcare advice when breast feeding became difficult versus controls 25 (62.5%) (P=0.02).
Findings on knowledge, indicate that all mothers in both groups knew that breastmilk was the first food for newborns. More participants from the intervention group gave correct responses to the rest of the nine questions compared to the control group but differences were not statistically significant.
In terms of attitudes towards IYCF practices, most of the mothers in both groups felt it was good to breastfeed exclusively (92.5%) and on demand (93.75%), that is, feeding on-cue. Almost all mothers (98.75%) in both groups had confidence in breastfeeding their child but the attitude towards expressing breast milk was varied. While 51% mothers felt confident to express breastmilk, 27.5% reported that they were not confident and 21% were not sure. The baseline results showed that about 30% of mothers considered breastmilk as child’s food even when they were away but only 10% actually followed and used expressed breastmilk in a cup. There were no significant differences in the responses between the intervention and control groups.
Infant Feeding Practices, Knowledge and Attitudes (6-23 Months)
Minimum meal frequency (MMF) was met by 79 (89%) children from the intervention group and 66 (83%) from the control group. Out of 82 children from the intervention group, 31 (38%) met the minimum dietary diversity score (MDD) and only 24 (30%) from the control group. A total of 53 children in both groups had a minimum acceptable diet with 31(38%) from the intervention group and 22 (29%) from the control. Despite the intervention group having a higher percentage of all the child feeding indicators (MMF, MDD and MAD), there were no statistically significant differences between the two groups.
In terms of knowledge, the majority 133/162 (82.1%), of the mothers in both the intervention and control group knew that children were to be breastfed beyond six months up to two years or more. Although not significant (P>0.05), more participants from the intervention group gave correct responses compared to the control group for all the other questions.
The majority of mothers with children 6-23 months had a positive attitude towards proper nutrition-related practices regarding infant feeding. Participants,153/162 (94.44%), felt that it was beneficial and good to feed a child with a diverse diet and continue breastfeeding a child beyond 6 months. Out of the 162 participants, almost all, 145 (92.6%) reported confidence in preparing a meal for their child. Also 125/162 (89.5%) of participants felt it was good to feed a child frequently. In addition, the majority of the participants reported it was not difficult to continue breastfeeding beyond 6 months and feed a child frequently. There were no statistical significant differences in the responses between the intervention and control groups.
Association between Knowledge and Attitudes to Feeding Practices
The association test showed that mothers who expressed difficulty in practicing EBF were likely not to practice EBF (P=0.006). Table 3 describes the relationship between knowledge variables and exclusive breastfeeding practices among mothers with children 0-6 months of age. The multivariate analysis showed that the odds of participants in the intervention to practice EBF was 0.9 times less compared to the controls (OR 0.90 [95% CI: 0.02 – 0.51] with P=0.006). These results show that there were differences between the two arms of the study with regards to their impact on exclusive breastfeeding feeding practices.
Table 3.Relationship between knowledge variables and exclusive breastfeeding practice among mothers with children 0-6 months in an intervention study in Nairobi urban informal settlements (N=80)
| Unadjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value | |
|---|---|---|---|---|
| Intervention | 0.09 [0.03 – 0.38] | 0.001 | 0.08 [0.02 – 0.46] | 0.004 |
| Meaning of exclusive breast feeding | 0.19 [0.05 – 0.67] | 0.010 | 0.28 [0.94 – 1.14] | 0.082 |
| Breastmilk is sufficient | 0.50 [0.18 – 1.38] | 0.181 | 0.46 [0.15 – 1.46] | 0.188 |
| Frequency of feeding | 0.29 [0.08 – 1.15] | 0.079 | 0.36 [0.08 – 1.52] | 0.164 |
| Benefits of exclusive breast feeding (babies) | 0.51 [0.08 – 3.28] | 0.477 | 0.18 [0.02 – 1.75] | 0.138 |
| Benefits of exclusive breast feeding (mothers) | 1.36 [0.49 – 3.75] | 0.556 | 1.49 [0.48 – 4.67] | 0.486 |
| Maintaining breastmilk supply | 1.45 [.015 – 13.8] | 0.744 | 1.14 [0.09 – 14.1] | 0.919 |
| Overcoming barriers to breastfeeding | 0.36 [0.09 – 1.35] | 0.129 | 0.19 [0.03 – 1.04] | 0.070 |
| Seeking healthcare | 0.85 [0.28 – 2.59] | 0.778 | 0.73 [0.19 – 2.79] | 0.643 |
Univariate regression analysis, level of significance (*P < 0.05), controlling for age of the caregiver, their educational level and age of the child.
Discussion
Contrary to our hypothesis that caregivers from the intervention group would have significantly better results in terms of babies who were exclusively breastfed, this study showed the practice of exclusive breastfeeding to be higher in the control group compared to the intervention group. According to Kenya Demographic Health Survey (KDHS) [4], EBF rate in Kenya was at 61% which is slightly higher than the intervention group (55%) but lower than the control group (92.5%). An additional study conducted in an urban informal settlement in Nairobi reported EBF rate to be 15.6% even after interventions that included facility-based and home-based counselling [35]. Even lower numbers were reported in another urban informal settlement in Nairobi that recorded a baseline EBF rate of 2% which improved to 55% similar to this current study’s intervention group after implementation of a home-based counselling program by community health workers [6]. Urban slum populations are growing rapidly and face unique challenges such as crowded living spaces, inadequate food, water, shelter, informal work sector as well as poor sanitation and hygiene. These challenges contribute to the populations having difficulties in meeting infant and young child feeding recommendations such as exclusive breastfeeding.
One of the possible reasons for the unexpected results of this study regarding the effectiveness of the nutrition education videos may be related to the setup of the clinics. In the intervention, during the video sessions, there were numerous activities occurring simultaneously. It was a noisy environment with a lot of conversations and ‘catching up’ amongst mothers along with children crying. The waiting area had limited space with some waiting outside since it was a high density facility with over 300 mothers visiting the clinic. This made it difficult for some of the mothers to concentrate during the video sessions. Those waiting outside due to limited space on the benches inside missed the videos. Crowded conditions might have limited participation if mothers were not confident enough to ask questions in such a public space. The high number of mothers being served at the clinic was expected because of the high number of people in the area. With high rates of urban migration and people looking for employment, the urban informal settlements in Nairobi including Mathare are growing at a rapid rate [36]. Another possible reason is that the messages should be provided to the mothers from delivery and if possible even during pregnancy. However, this was a short study that did not follow mothers continuously from pregnancy to the child’s second birthday. The short time frame also may have not allowed for mothers to apply the knowledge gained and realize behavior change. These results emphasize that an increase in knowledge does not translate to adoption of practices, and the extra effort needed to realize behavior change among mothers was not obtained.
Generally, mothers were knowledgeable about breastfeeding. For example, they knew that breastmilk was important for infant growth and development. Similarly, a study conducted in two urban informal settlements in Nairobi, Kenya showed that some of the positive beliefs that mothers had towards breastfeeding included its association with good health of a child [37]. Results from this study showed that most mothers were also aware that breastmilk could be expressed but very few practiced this strategy. Lack of confidence and low acceptance of the practice was accompanied by the attitude that it might hinder EBF. According to the Kenyan Ministry of Health, freshly expressed breastmilk can be stored at room temperature if used within 8 hours [38]. This practice could be useful for working mothers in the urban informal settlements leaving children under care of someone else. A study carried out in Mississippi, USA reported barriers to exclusive breastfeeding at baseline that included pumping breast milk. An innovative video was used as an intervention which resulted in improved perceptions regarding the practice [39]. This is an indication that videos followed by interactions or discussions with peers can improve mothers’ perceptions towards expressing and storing breastmilk.
In line with our hypothesis on complementary feeding practices, the intervention group was generally better than the control group in terms of the 3 child feeding indicators. Kenyan data for 2014 [4], report only 51% of children met MMF, 41% MDD and 22% MAD. Fewer mothers met MMF and MDD in the national survey when compared to our study sample. Similarly, a study conducted in informal urban settlements of Nairobi [40] reported higher rates of recommended practices in the intervention group which received home-based nutrition counselling compared to the control group using the same indicators; MMF (80.7% vs 74%), MDD (42.9% vs 38.9%), MAD (27.6% vs 26.5%). A cross-sectional analytical research study conducted in Korogocho urban informal setllements of Nairobi [7] also reported 88.3% of the participants attaining MMF, 17.9% MDD and 15.4% attaining MAD. The challenges facing urban informal settlements’ dwellers regarding food insecurity could contribute to the difficulties in meeting MAD for children in these areas.
This study targeted mothers but in cases where a mother was accompanied by the father of the child to the clinic, both could potentially benefit. However, this was very rare and in the vast majority of cases it was only the mother who came with the child to the clinic. If alternative strategies are adopted in the future such as home visits, then fathers could be included in the interventions along with other influential family members like mothers-in-law and grandmothers. Several studies have shown effectiveness of including fathers in promoting exclusive breastfeeding and complementary feeding practices [9,10,34,45].
The importance of having professionals as well as peer support in promoting EBF has been well documented [8-10,43]. A study done in a poor peri-urban area of Peru trained health workers to teach mothers key messages that were simple, standard and age-specific and additionally provided them with other educational materials, such as fliers. There was improvement in the knowledge of mothers along with better child feeding practices [44]. The use of age-specific videos to a targeted audience might be more effective than the approach used in the current study where all mothers were seated in one waiting area watching the same videos regardless of the child’s age. Videos are a good teaching aid but it appears that the direct contact/discussions the mothers had with a health worker was more effective. This is similar to a review paper which reported that educating a group of women had little impact unless it was interactive [8]. Another study in Singapore [45] showed that mothers who received both educational material and individual counselling, practiced more EBF than those who received only educational material [43]. Having more time for discussions and interactions after watching the videos would possibly have been more useful to the mothers. It is also important for health workers to provide an environment for mothers to feel more motivated regarding infant and young child feeding by increasing their autonomy, competence and relatedness. To achieve this, further measures are necessary such as training health workers on practical and emotional support of the mothers which is limited in Kenyan hospital staff [27].
Different strategies have been adopted for designing interventions with the purpose of promoting EBF; Baby Friendly Hospital Initiatives (BFHI), the Baby Friendly Community Initiatives (BFCI) [12,46], and integrated community-based interventions. A review on EBF showed that the most effective strategy was a combination of hospital-based and community-based interventions [10]. It is possible that better results would have been achieved if this study had incorporated a different strategy or delivery method using an intervention package that might be extended into the community and include home visits by community health workers. A Kenyan study that adopted home-based nutrition counselling showed positive results on EBF rates in study participants [6]. Peer support has also been shown to be effective in behavior change [47,48]. An additional behavior change communication study used educational videos, but divided the target group into smaller units where they could watch and discuss the videos amongst themselves. This led to significant changes in IYCF practices [24]. Peer-to-peer learning and support could be considered as an additional approach to encourage discussions among mothers.
A number of limitations may have impacted the outcomes of the current study. The design was post-intervention cross sectional which lasted for a relatively short time thus making it challenging to achieve significant behavioral change. The intervention delivery strategy may not have allowed mothers to watch all the videos during their visits in the 3-4 months that the videos were shown. Also, they may have watched videos that did not target the age of their children. In addition, the two clinics had differences in organization and resources. Mathare North had little space and not all mothers were able to sit in the waiting room during the health and nutrition talks. In Kahawa West however, the structure was more spacious and it was more likely that all the mothers sat in the waiting room and thus could attend and listen to health and nutrition talks. This reflects a relative advantage of a more appropriate physical setting available to the control group compared to the intervention group. It should be noted that there was also limited staff in the intervention facility in Mathare North, which limited in-person interactions with the patients. In a systematic review it was reported that most successful interventions were those that followed women from pregnancy to lactation and included interactive sessions throughout [8]. This combined approach might be a superior delivery strategy, allowing for sufficient time for behavior change and adoption of practices by mothers in the urban informal settlements and not just increased knowledge regarding nutrition.
Conclusions and Recommendations
This study highlights the inadequacy in optimal IYCF practices in urban informal settlements’ populations. Children living in urban informal settlements are likely to face food insecurity and not meet the minimum standards of EBF for 6 months and a minimum acceptable diet after 6 months. This calls for interventions that can contribute to improved practices in these populations allowing for optimal growth and development of the child. Unfortunately, the intervention in this study did not have positive significant results for important indicators like EBF and MAD. There was a generally high nutrition knowledge, positive attitude and complementary feeding indicators were better in the intervention group though not a statistically significant result. Interventions that combine delivery strategies such as home-based counselling and facility-based counselling may be a better approach for improving IYCF in the urban informal settlements of Nairobi. Increased contact of healthcare providers with caregivers, along with interaction and peer support appear to have greater impact than the strategy of only using video messages for nutrition education combined with limited discussions.
Acknowledgements
Special appreciation goes to the Hebrew University of Jerusalem, Kenyatta University, Kenya Ministry of Health, Mathare North and Kahawa West Health Centers’ staff members and all the caregivers who participated in the study.
Financial Support
Ms. Patricia Kiprono was sponsored by a grant from the Pears Foundation, UK to conduct this study in Kenya.
Conflict of Interest
None
References
1. WHO.Infant mortality. WHO [Internet]. 2018 [cited 2018 Oct 14]; Available from: http://www.who.int/gho/child_health/mortality/neonatal_infant_text/en/
2. UNICEF. Multi-sectoral Approaches to Nutrition. 2013;1–4.
3. UNICEF, WHO, World Bank Group, United Nations. Levels and Trends of Child Mortality. 2018.
4. Kenya Demographic and Health Survey, KDHS. Kenya [Internet]. 2014. Available from: https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf
5. Njoroge NM, Munene F. Nutrition survey conducted in the slums of Nairobi County [Internet]. 2017. Available from: http://www.nutritionhealth.or.ke/wp-content/uploads/SMART Survey Reports/Nairobi County SMART Survey Report - May 2017.pdf
6. Kimani-Murage EW, Griffiths PL, Wekesah FM, et al. Effectiveness of home-based nutritional counselling and support on exclusive breastfeeding in urban poor settings in Nairobi: A cluster randomized controlled trial. Global Health. 2017;13(1):1–16.
7. Korir J. Determinants of complementary feeding practices and nutritional status of children 6-23 months old in Korogocho slum, Nairobi County, Kenya. [Dissertation]. Kenyatta University. 2013.
8. Hannula L, Kaunonen M, Tarkka MT. A systematic review of professional support interventions for breastfeeding. J Clin Nurs. 2008;17(9):1132–43.
9. Chapman DJ, Morel K, Anderson AK, et al. Review: Breastfeeding peer counseling: From efficacy through scale-up. J Hum Lact. 2010;26(3):314–26.
10. Kim SK, Park S, Oh J, et al. Interventions promoting exclusive breastfeeding up to six months after birth: A systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2018;80:94–105. Available from: https://doi.org/10.1016/j.ijnurstu.2018.01.004
11. Miller JD, Young SL, Boateng GO, et al. Greater household food insecurity is associated with lower breast milk intake among infants in western Kenya. Matern Child Nutr. 2019;15(4):1–8.
12. Maingi M, Kimiywe J, Iron-Segev S. Effectiveness of Baby Friendly Community Initiative (BFCI) on complementary feeding in Koibatek, Kenya: A randomized control study. BMC Public Health. 2018;18(1):1–11.
13.Lassi ZS, Das JK, Zahid G, et al. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: A systematic review. BMC Public Health. 2013;13(SUPPL.3):S13. doi: 10.1186/1471-2458-13-S3-S13.
14. Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health [Internet]. 2011;11 Suppl 3(Suppl 3):S25. doi: 10.1186/1471-2458-11-S3-S25.
15. Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr. 2008; 4: 24–85.
16. World Health Organisation WHO. Baby-friendly Hospital initiative : revised, updated and expanded for integrated care. Section 4, Hospital self-appraisal and monitoring [Internet]. World Health Organization. 2009. Section 4. Available from: http://apps.who.int/iris/bitstream/handle/10665/43593/9789241594998_eng.pdf;jsessionid=2BC14F0F061A6BA487D60B80D91271C1?sequence=7
17. Mbogori T, Murimi M. Effects of a Nutrition education intervention on maternal knowledge, child care practices and nutrition status. J Nutr Educ Behav. 2016;48(7):S3. doi: https://doi.org/10.18203/2394-6040.ijcmph20191798
18. Mitchell-Box KM, Braun KL. Impact of male-partner-focused interventions on breastfeeding initiation, exclusivity, and continuation. J Hum Lact. 2013;29(4):473–9.
19. Davidson EL, Ollerton RL. Partner behaviours improving breastfeeding outcomes: An integrative review. Women and Birth. 2020;33(1):e15–23.
20. Abbass-Dick J, Brown HK, Jackson KT, et al. Perinatal breastfeeding interventions including fathers/partners: A systematic review of the literature. Midwifery. 2019;75:41–51.
21. Zelenko O, Mulugeta A, Gallegos D. A cross-sectional comparison of breastfeeding knowledge, attitudes, and perceived partners’ support among expectant couples in Mekelle Ethiopia. Int Breastfeed J. 2020.
22. Nguyen PH, Frongillo EA, Sanghvi T, et al. Engagement of Husbands in a Maternal Nutrition Program Substantially Contributed to Greater Intake of Micronutrient Supplements and Dietary Diversity during Pregnancy: Results of a Cluster-Randomized Program Evaluation in Bangladesh. J Nutr [Internet]. 2018;(4).
23. Nguyen PH, Kim SS, Sanghvi T, et al. Integrating nutrition interventions into existing maternal, neonatal, and child health program increased maternal dietary diversity, micronutrient intake, and exclusive breastfeeding practices in Bangladesh: Results of a cluster-randomized program evaluation. J Nutr. 2017;147:2326-2337.
24. SPRING. Using a communication-led video approach to promote maternal, infant, and young child nutrition in Odisha, India. 2014;(September).
25. Zhou A, Ni B. Knowledge , attitudes , and practice ( KAP ) survey and barrier analysis for infant and young child feeding practices Sittwe and Pauktaw townships , Rakhine State – Republic of the Union of Myanmar {Internet}. 2015. Available from: https://themimu.info/sites/themimu.info/files/documents/Report_Nutrition_KAP_BA_Rakhine_SCI_Jun2015.pdf
26. UNICEF. The Community Infant and Young Child Feeding Counselling Package [Internet]. 2013. Available from: http://www.unicef.org/nutrition/files/Key_Messages_Booklet_for_counselling_cards.pdf
27. Schneider L, Ollila S, Kimiywe J, et al. Is competence enough to enable Kenyan mothers to make good infant and young child feeding decisions? Matern Child Nutr. 2017;13(4):1–9.
28. Pelto GH, Martin SL, van Liere MJ, et al. Perspectives and reflections on the practice of behaviour change communication for infant and young child feeding. Matern Child Nutr. 2016;12(2):245–61.
29. Yamane T. Statistics, An Introductory Analysis, 2nd Ed., New York: Harper and Row. 1967.
30. WHO, Profiles C, WH0. Indicators for assessing infant and young child feeding practices. Young [Internet]. 2010;2007:1–19. Available from: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Indicators+for+assessing+infant+and+young+child+feeding+practices#0
31. WHO & UNICEF. Indicators for assessing infant and young child feeding practices. Vol. 2007, World Health Organization. 2008.
32. Ochola S. Maternal Infant and Young Child Nutrition ( Miycn ) Knowledge , Attitudes , Survey Report Samburu County. 2018.
33. Macias YF, Glasauer P. Guidelines for assessing nutrition-related Knowledge, Attitudes and Practices manual [Internet]. Food and Agriculture Organization of the United Nations. 2014. 1–180 p. Available from: www.fao.org/docrep/019/i3545e/i3545e00.htm
34. World Health Organization. Interpretation Guide Nutrition Landscape Information System (NLIS). Who [Internet]. 2010;1–51. Available from: https://apps.who.int/iris/handle/10665/44397
35. Ochola SA, Labadarios D, Nduati RW. Impact of counselling on exclusive breast-feeding practices in a poor urban setting in Kenya: A randomized controlled trial. Public Health Nutr. 2013;16(10):1732–40.
36. United Nations Human Settlements Programme (UN-HABITAT). Nairobi Urban Sector Profile [Internet]. 2006. Available from: https://unhabitat.org/sites/default/files/download-manager-files/Kenya Nairobi Urban Profile.pdf
37. Wanjohi M, Griffiths P, Wekesah F, et al. Sociocultural factors influencing breastfeeding practices in two slums in Nairobi, Kenya. Int Breastfeed J. 2017;12(1):1–8.
38. Ministry of Health Kenya. Guidelines for securing a breastfeeding friendly environment at the work place [Internet]. 2018.
39. Khoury AJ, Mitra AK, Hinton A, et al. An innovative video succeeds in addressing barriers to breastfeeding among low income women. J Hum Lact. 2002;18(2):125–31.
40. Macharia TN, Ochola S, Mutua MK. Association between household food security and infant feeding practices in urban informal settlements in Nairobi , Kenya. J Dev Orig Health Dis. 2019;9(2018):20–9.
41. Wolfberg AJ, Michels KB, Shields W, et al Dads as breastfeeding advocates: Results from a randomized controlled trial of an educational intervention. Am J Obstet Gynecol. 2004;191(3):708–12.
42. Susin LRO, Giugliani ERJ. Inclusion of fathers in an intervention to promote breastfeeding: Impact on breastfeeding rates. J Hum Lact. 2008;24(4):386–92.
43. Gross SM, Caulfield LE, Bentley ME, et al. Counselling and motivational videotapes increase duration of breast- feeding in Africa-American WIC participants who initiate breast-feeding.
44. Penny ME, Creed-Kanashiro HM, Robert RC, et al. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: A cluster-randomised controlled trial. Lancet. 2005;365(9474):1863–72.
45. Mattar CN, Chong Y, Chan Y, et al. Simple antenatal preparation to Improve breastfeeding practice. Obstet Gynecol. 2007;109(1):73–9.
46. Kimani-Murage EW, Kimiywe J, Kabue M, et al. Feasibility and effectiveness of the baby friendly community initiative in rural Kenya: Study protocol for a randomized controlled trial. Trials [Internet]. 2015;16(1).
47. Chepkirui D, Nzinga J, Jemutai J, et al. A scoping review of breastfeeding peer support models applied in hospital settings. Int Breastfeed J. 2020;15(1):1–11.
48. Kabakian-Khasholian T, Nimer H, Ayash S, et al. Experiences with peer support for breastfeeding in Beirut, Lebanon: A qualitative study. PLoS One. 2019;14(10):p.e0223687.
Received: January 16, 2023;
Accepted: February 20, 2023;
Published:February 22, 2023 .
To cite this article : Kiprono PJ, Kimiywe J, Iron-Segev S. Impact of Nutrition Education Videos on Child Feeding Practices in Urban Informal Settlements of Nairobi. Health Education and Public Health. 2023; 7(1): 517-525. doi: 10.31488/HEPH.180.
© 2023 Kiprono PJ, et al.
