Research Article / Open Access
DOI: 10.31488/HEPH.177
Longitudinal Change in The Cumulative Incidence and Maintenance Rate of Metabolic Syndrome among Participants of the Specifific Health Check and Guidance System in Japan
Iseki K 1,2,3, Konta T1, Asahi K1, Fujimoto S1, Moriyama T1, Yamagata K1, Tsuruya K1, Narita I1, Kondo M1, Kasahara M1,Shibagaki Y1, Iseki C3, Watanabe T1
1. The Japan Specific Health Checkups study (J-SHC study) Group, Japan
2. Clinical Research Support Center, Nakamura Clinic, Japan
3. Okinawa Renal and Heart Association (OHRA), Japan
*Corresponding author:Dr. Kunitoshi Iseki, Clinical Research Support Center, Nakamura Clinic 4-2-1 Iso, Urasoe, Okinawa 901-2132, Japan; Tel: 098-870-6600, Fax: 098-870-6604
Abstract
Background: The trends in cumulative incidence and maintenance rate of metabolic syndrome (MetS) are not yet available in Japan. Methods: Data of the Tokutei-Kensin from 2008 to 2014 were used in this study. The total number of participants was 3,809,853. Among them, we identified 933,490 individuals who have screened at least twice during the study period. The mean number of visits was 3.4 times per person. Cumulative incidence of MetS was defined among those who were free of MetS at the first screening. The maintenance rate of MetS was defined among those who were diagnosed with MetS at both the first and the second screening. Kaplan Meier curves were obtained for both the incidence and maintenance rate of MetS.Results: The cumulative incidence of MetS was 5.7%, 9.6%, 3.5% (1 year), 8.0%, 12.4%, 5.3% (2 years), 8.5%, 12.8%, 5.8% (3 years), 8.0%, 12.3%, 5.4% (4 years), 9.6%,16.2%, 5.4% (5 years), and 7.0%, 14.7%, 3.0% (6 years), in total, men, and women, respectively. The maintenance rate of MetS was 47.4%, 49.7%, 43.4% (1 year), 44.6%, 46.9%, 39.8% (2 years), 42.7%, 44.5%, 39.8% (3 years), 42.4%, 45.1%, 38.5% (4 years), 38.9%, 38.1%, 40.1% (5 years), and 40.0%, 35.3%, 46.2% (6 years), in total, men, and women, respectively. Incidence of MetS was higher in men than that of women. However, the maintenance rate of MetS was similar between men and women. Conclusions: Maintenance rate of MetS has decreased substantially in both genders who were diagnosed with MetS at the initial screening. However, the actual number of MetS has increased as the higher numbers of subjects developed MetS after the screening.
Keywords: metabolic syndrome, cumulative incidence, maintenance rate, gender difference, life expectancy
Introduction
Metabolic syndrome (MetS) and obesity have been known as related to cardiovascular disease in western countries [1, 2]. Obesity was not so common among Japanese, in particular women, Also, the incidence of cardiovascular disease is relatively low among Japanese [3]. A recent literature review supports the positive relationship between MetS and cardiovascular disease [4].
A specific nationwide health check-up and guidance system, called Tokutei-Kenshin, was initiated in April 2008 in Japan [5]. This project aims to detect metabolic syndrome (MetS) and if confirmed, to provide individual instruction to modify lifestyle and the necessary treatment. The target population comprises Japanese citizens between the ages of 40–74 years. We have been focused mostly on chronic kidney disease (CKD) [6, 7, 8], diabetes mellitus (DM) [9, 10], and mortality [11-14]. Lifestyle is a significant modifier of CKD [15], cardiovascular disease (CVD) [16], and mortality [16, 17]. We recently confirmed that MetS was a significant risk factor for mortality [18].
Intervention through this screening program was shown to be very effective for the reversal of MetS [19]. However, the proportion of people attending the intervention program is as low as 11%. The trends in the cumulative incidence and maintenance rate of MetS have not been well studied. Such information would be helpful for the future modification of the protocol of screening among the Japanese population. However, lifestyle modification should be carefully performed such as educational attainment and marital status [20], gender difference [21], uric-acid level [22], and smoking habit [23].
In the present study, we examined the MetS in both cumulative incidence and maintenance rate among the subjects who have participated, in at least twice the nationwide screening.
Methods
Study subjects and baseline characteristics
Details of the dataset of the nationwide screening program of the Specific Health Check-up and Guidance System (Tokutei-Kensin) in Japan have been previously published [6-18]. From 2008 to 2014, we collected individual records of 3,809,853 participants from 192 municipals of 27 prefectures. The process for the database construction is summarized in Figure 1. From the total number of subjects who participated (about 3.8 million), we selected those who visited at least twice during the study visit. Finally, we used the dataset of 933,490 participants for the analysis. During the study period, the mean number of visits was 3.4 times per subject. MetS was defined as waist circumference (men≥85cm, women≥90cm) plus two or three abnormal values in blood sugar metabolism (fasting blood glucose≥100mg/dL or HbA1c≥5.2% by 2012 (JDS), HbA1c≥5.6% by NGSP since 2013), lipid (triglyceride≥150mg/dL, or HDL cholesterol<40mg/dL), and blood pressure (systolic≥130mmHg, or diastolic≥85mmHg) [18]. The original database was solely used and managed by Okinawa Heart and Renal Association (OHRA). Furthermore, the preliminary dataset was verified and confirmed independently by Dr. Tsuneo Konta. Afterward, further analyses were done by using a standard analysis file (SAF) without any personal identifier. We used data from 2008-2014; for Multivariate Cox regression analysis with MetS new-onset and MetS maintenance at 1 year as the outcome, the baseline subjects were those who were first seen in 2008-2013, and the outcome was the new-onset of MetS and the maintenance of MetS at 1 year.
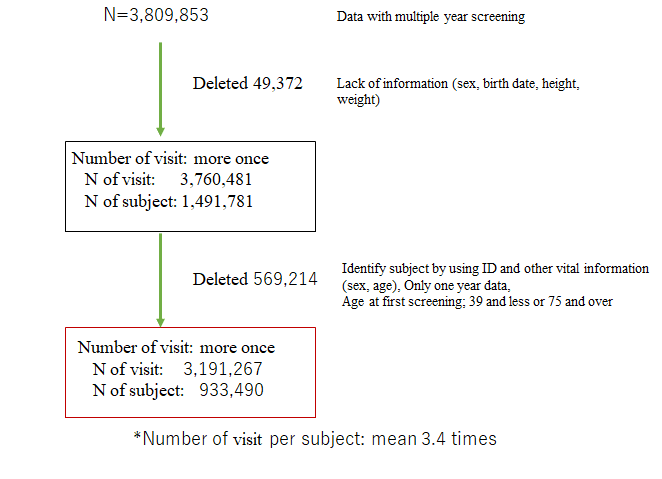
Figure 1:
Table 1:Number of subjects used for the incidence curve by Kaplan Meier analysis
| MS Incidence | Men | Women | Men, Age≥65 | Men, Age<65 | Women, Age≥65 | Women, Age<65 |
|---|---|---|---|---|---|---|
| Baseline | 278123 | 474686 | 146415 | 131708 | 229630 | 245056 |
| 1-year | 278123 | 474686 | 146415 | 131708 | 229630 | 245056 |
| 2-years | 186095 | 337062 | 94440 | 91655 | 155254 | 181808 |
| 3-years | 125851 | 247816 | 62404 | 63447 | 110515 | 137301 |
| 4-years | 76203 | 163106 | 36923 | 39280 | 70241 | 92865 |
| 5-years | 26544 | 60865 | 13096 | 13448 | 26003 | 34862 |
| 6-years | 3464 | 8388 | 1710 | 1754 | 3434 | 4954 |
Table 2:Number of subjects used for the maintenance rate curve by Kaplan Meier analysis
| MS Maintenance | Men | Women | Men, Age≥65 | Men, Age<65 | Women, Age≥65 | Women, Age<65 |
|---|---|---|---|---|---|---|
| Baseline | 54980 | 32827 | 29019 | 25961 | 18937 | 13890 |
| 1-year | 54980 | 32827 | 29019 | 25961 | 18937 | 13890 |
| 2-years | 26043 | 14723 | 13359 | 12684 | 8155 | 6568 |
| 3-years | 12494 | 6876 | 6259 | 6235 | 3714 | 3162 |
| 4-years | 5421 | 2941 | 2644 | 2777 | 1542 | 1399 |
| 5-years | 1473 | 804 | 704 | 769 | 403 | 401 |
| 6-years | 97 | 41 | 53 | 44 | 23 | 18 |
All procedures performed in studies involving human participants were performed following the ethical standards of the institutional and/or national research committee at which the studies were conducted (Fukushima Medical University; IRB approval number #1485, #2771) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was performed according to Ethical Guidelines for Medical and Health Research Involving Human Subjects enacted by MHLW of Japan
In the context of the guideline, the investigators shall not necessarily be required to obtain informed consent, but we made public information concerning this study on the web [http://www.fmu.ac.jp/univ/sangaku/data/koukai_2/2771.pdf] and ensured the opportunities for the research subjects to refuse to utilize their personal information.
Calculation of cumulative incidence of MetS
The denominator is the number of people in each year group between the first and second checkup among those with MetS (-) at the first checkup (the number in the 1-year group is the number of people whose interval between the first and second checkups was 1 year), and the numerator is the number of new cases of MetS among them.
Calculation of the maintenance rate of MetS
Among the subjects with MetS (+) at the first checkup, and the rate of maintenance of MetS (+) at the time of the next checkup. The denominator is the number of people who were MetS (+) at the first checkup and the number of people in each year group between the first and second checkups (the number of people in the 1-year group is the number of people whose interval between the first and second checkups was 1 year), and the numerator is the number of people who maintained MetS (+) at the second checkup.
Statistical analyses
Data were analyzed with SAS/STAT software (version 6.03, SAS Institute, Tokyo, Japan). The student's t-test and the Chi-squared test were performed to compare the significance of discrete variables. Multivariate Cox regression analysis was performed to evaluate the risks for the changes in the trend of the cumulative incidence and maintenance rate of MetS. Factors used for the adjustment were body mass index, systolic and diastolic blood pressure, fasting blood glucose, HbA1c, triglyceride, HDL cholesterol, LDL cholesterol, eGFR, proteinuria, alcohol intake, smoking, history of stroke, acute myocardial infarction renal failure, dialysis, and drug use for hypertension, diabetes mellitus, and hyperlipidemia and were based on self-reported information in the medical questionnaire. The hazard ratio and 95% confidence interval were obtained. A P value of less than 0.05 was considered statistically significant in all analyses. We also examined the Kaplan Meier curves for the cumulative incidence of MetS and maintenance rate of MetS. The number of subjects used for the Kaplan Meier curves were shown in Tables 1 and 2.
Results
The cumulative incidence of MetS
As a whole, the cumulative incidence of MetS was 6.2% (total), 10.1% (men), and 3.9% (women), respectively. The relationship between the cumulative incidence of MetS and the interval of screening was shown up to 6 years (Figure 2), it was gradually increased. In particular, the cumulative incidence in men was higher than that of women. Baseline characteristics of subjects who remained without MetS and developed MetS were summarized in (Supplementary Table 1). Those who developed MetS were a significantly higher proportion of men of older age. Other variables except renal failure/ dialysis were also significantly different as the number of subjects was large.
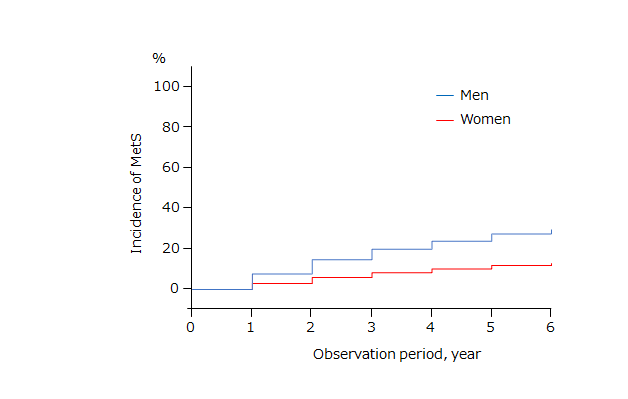
Figure 2:Kaplan-Meier curve: Incidence of metabolic syndrome among those who were free of metabolic syndrome at the first screening
The maintenance rate of MetS
It was 46.6% (total), 48.9% (men), and 38.5% (women), respectively. Similar to the changes in cumulative incidence, the relationship between the maintenance rate of MetS and the interval of screening is shown up to 6 years. (Figure 3). After the initial screening, the maintenance rate of MetS gradually declined. Baseline characteristics of subjects who remained MetS and disappeared MetS were summarized in (Supplementary Table 2). Those who remained MetS were a significantly higher proportion of men of older age. Other variables except for current smokers and history were also significantly different.
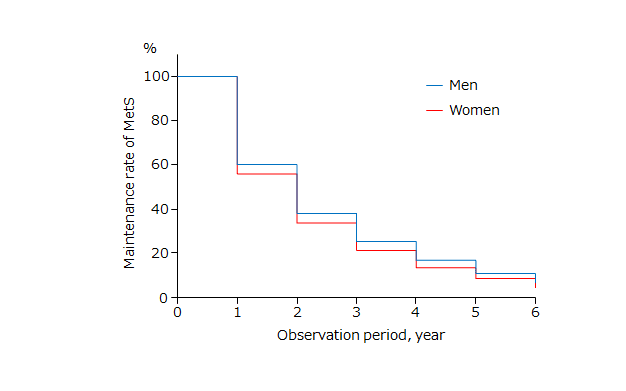
Figure 3:Kaplan-Meier curve: Maintenance rate of metabolic syndrome among those subjects who were diagnosed metabolic syndrome at the first screening
Table 3:The association of age, gender with the cumulative incidence and maintenance rate of MetS status at 1-year
| Cumulative Incidence of MetS | Maintenance rate of MetS | |||
|---|---|---|---|---|
| Variables | Unadjusted HR (95%CI) | Adjusted HR (95%CI)* | Unadjusted HR (95%CI) | Adjusted HR (95%CI)* |
| Men (vs. Women) | 2.90 (2.83-2.96) | 2.38 (2.29-2.47) | 1.29 (1.25-1.33) | 1.43 (1.37-1.51) |
| < 65 years (vs. <65 years) | 1.17 (1.15-1.20) | 1.35 (1.31-1.39) | 1.09 (1.06-1.12) | 1.10 (1.05-1.14) |
*Factors used for adjustment; body mass index, SBP, DBP, FBS, HbA1c, TG, HDL-C, LDL-C, eGFR, proteinuria, alcohol intake, smoking, past history of stroke, acute myocardial infarction renal failure, dialysis, and drug use for hypertension, diabetes mellitus, and hyperlipidemia
Effect of gender and age on the cumulative incidence and maintenance rate of MetS
By using a multivariate Cox hazard analysis, the multivariate-adjusted hazard ratio (HR) of cumulative incidence of MetS was significantly higher in men; HR was 2.38 (95% confidence interval 2.29-2.47), and elderly (age≥65 years); HR was 1.35 (95% confidence interval 1.31-1.39), respectively (Table 3). The cumulative incidence of MetS was 5.7% (age< 65 years) and 6.6% (age≥65 years). The multivariate-adjusted hazard ratio (HR) of the maintenance rate of MetS was significantly higher in men; HR was 1.43 (95% confidence interval 1.37-1.51), and elderly (age≥65 years); HR was 1.10 (95% confidence interval 1.05-1.14), respectively. Maintenance rate of MetS was 45.5% (age< 65 years) and 47.5% (age≥65 years). Kaplan Meier curves were shown in Supplementary Figures 1 and 2.
Baseline characteristics by gender
They were shown in Supplementary Table 3. In men, the prevalence of smokers, DM, and history of CVD and stroke were more than twice as high compared to women. However, the current smoker was less in the elder-age group (≥65 years) than in men (Supplementary Table 4). In women, the current smoker was also higher among the younger age group (<65 years) (Supplementary Table 5).
Discussion
This study examined the cumulative incidence and maintenance rate of MetS among the nationwide screening program from the fiscal year 2008 to 2014 (6 years). Men and the elderly group (age≥65) population were at risk of higher cumulative incidence and maintenance rate of MetS. According to the abridged life table from the Ministry of Health, Labour and Welfare, the life expectancy was78.4 years in men and 85.3 years in women in 2002, and it increased to 81.4 in men and 87.5 years in 2019, respectively. The gender discrepancy in life expectancy remains high at 6 years, yet the reasons are not clear. Early detection of MetS and lifestyle modification may improve life expectancy in men.
Subjects with MetS have a significant impact on the incidence of CKD [6, 7, 8], diabetes mellitus (DM) [9, 10], and mortality [11-14]. Accordingly, when diagnosed MetS, they are entitled to further examination and lifestyle intervention. Lifestyle per se is a significant modifier of CKD [15], CVD [16], and mortality [16-17]. Recently, we confirmed that MetS was a significant risk factor for mortality [18]. Therefore, early intervention in overweight/obese adults, namely MetS subjects is necessary to prevent the progression of CKD [24, 25] and death.
The dipstick proteinuria test for CKD detection was cost-effective [26, 27], but not yet shown for the diagnosis of MetS at the general screening. The key strategy for the prevention of MetS is to keep body weight within the normal range through nutritional management and adequate exercise. in particular aged populations. Intervention through this screening program was shown to be very effective for the reversal of MetS [19]. However, the proportion of people attending the program is as low as 11%. The trends in the cumulative incidence and maintenance rate of MetS have not been well studied. Such information would be helpful for the future modification of the protocol of screening among the Japanese population.
Lifestyle modification if convinced by the screened participants would prevent the overall incidence of MetS and reduce the prevalence of MetS. Other than the weight reduction in overweight and obese subjects, excess alcohol intake, in particular, men, is frequently observed with MetS. Alkerwi A et al recommended restricting alcohol consumption to less than 20 g/day among women, and less than 40 g/day among men [28]. Also, special education is needed for smokers as cessation of smoking, prevalent among men, is an independent predictor of new-onset of MetS. [23] Other lifestyles such as depression [29] and self-reported sleep duration [30] are reported to the associated with MetS. These observations need to be confirmed among the Japanese but are suggesting the importance of further questionnaires among apparently healthy people.
MetS were defined as waist circumference (men≥85cm, women≥90cm) plus two or three abnormal values in blood sugar metabolism, lipid, and blood pressure [18]. Waist circumference is a surrogate of central obesity but is often variable by body size, gender, and race. We reported the significance of “a body shape index (ABSI)” on all-cause mortality among screened subjects [14]. ABSI seemed to be a better predictor of death than the body mass index (BMI). However, the presence of CKD affected differently on mortality between men and women.
Strengths and limitations
The strength of the present study is that we have followed many participants of the nationwide screening program. We believe that this cohort represents the currently available database for the analysis of the changes in MetS status in Japan.
There are several limitations in the present study. First, participants in this analysis were those who had an interest in lifestyle and their health conditions. The participation rate was 38.9% (2008) and 51.4% (2016) of the target population. (Ministry of Health, Labor and Welfare) Therefore, it would not be representative of the whole Japanese population. We have no data on whether the MetS (+) individuals had attended the intervention program or not. A previous study showed that men and relatively younger (age<65 years) had a lower participation rate compared to their counterparts [27]. Second, other socio-economic factors related to the incidence and prevalence of MetS are unknown in this screening program. The number of family members, the presence of a spouse, and the location of residence might influence the lifestyle. Third, factors other than the differences in lifestyles and history of CVD, stroke, and renal failure at baseline may explain the results of the present study. Long-term lifestyle would be difficult to change by a single intervention, in a particular elderly population. Fourth, we have no data on those aged 75 and over. The medical care system for the elderly in the later stage of life also started in 2009 in Japan. Further studies on transition to this program may be warranted. Finally, other limitations on the diagnosis of MetS have been discussed in the previous paper [18].
Conclusions
This study showed the cumulative incidence of MetS increased steadily after the screening. In particular, subjects aged (≥65) men were at risk of developing MetS. However, the maintenance rate of MetS has declined steadily even after 3 years after the screening.
Conflict of Interest
The authors state they have no Conflict of Interest (COI).
Financial Support
This study was supported by a Health and Labor Sciences Research Grant for Study on the design of the comprehensive health care system for chronic kidney disease (CKD) based on the individual risk assessment by Specific Health Checkup from the Ministry of Health, Labor and Welfare of Japan, a Grant-in-Aid for Research on Advanced Chronic Kidney Disease (REACH-J), practical Research Project for Renal Disease from Japan Agency for Medical Research and Development, AMED and JSPS KAKENHI Grant Number JP18K11131.
Acknowledgment
This study was not possible without the generous support from the public health nurses, KOKUHO agency in each district.
References
1. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119:812-819.
2. Müller MJ, Lagerpusch M, Enderle J, et al. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev. 2012;13:6-13.
3. Ueshima H. Explanation for the Japanese paradox: prevention of increase in coronary heart disease and reduction in stroke. J Atheroscler Thromb 2007;14:278-286.
4. Watanabe J, Kotani K. Metabolic Syndrome for Cardiovascular Disease Morbidity and Mortality Among General Japanese People: A Mini Review. Vasc Health Risk Manag. 2020;16:149-155.
5. Kohro T, Furui Y, Mitsutake N, et al. The Japanese National Health Screening and Intervention Program Aimed at Preventing Worsening of the Metabolic Syndrome. Int Heart J. 2008;49:193-203.
6. Iseki K, Asahi K, Moriyama T, et al. Risk factor profiles based on eGFR and dipstick proteinuria: Analysis of the participants of the Specific Health Check and Guidance System in Japan 2008. Clin Exp Nephrol. 2012;16:244-249.
7. Konta T, Ikeda A, Ichikawa K, et al. Blood pressure control in a Japanese population with chronic kidney disease: A baseline survey of a nationwide cohort. Am J Hypertens. 2012;25:342-347.
8. Tsuruya K, Yoshida H, Nagata M, et al. Impact of the triglycerides to high-density lipoprotein cholesterol ratio on the incidence and progression of chronic kidney disease: a longitudinal study in a large Japanese population. Am J Kidney Dis. 2015;66:972-983.
9. Kudo A, Asahi K, Satoh H, et al. Fast eating is a sole predisposing factor for new-onset diabetes: a report from a Japanese nation-wide cohort. Fast eating is a strong risk factor for new-onset diabetes among the Japanese general population. Sci Rep. 2019;9(1):8210.
10. Iwasaki M, Kudo A, Asahi K, et al. Fast walking is a preventive factor against new-onset diabetes mellitus in a large cohort from a Japanese general population. Sci Rep. 2021;11(1):716 9.
11. Iseki K, Konta T, Asahi K, et al. “Design of the comprehensive health care system for chronic kidney disease (CKD) based on the individual risk assessment by Specific Health Check.” Association of dipstick hematuria with all-cause mortality in the general population: Results from the Specific Health Check and Guidance Program in Japan. Nephrol Dial Transplant. 2018;33(5):825-832.
12. Iseki K, Konta T, Asahi K, et al. “Design of the comprehensive health care system for chronic kidney disease (CKD) based on the individual risk assessment by Specific Health Check.” Dipstick proteinuria and all-cause mortality among the general population. Clin Exp Nephrol. 2018;22(6):1331-1340.
13. Iseki K, Asahi K, Yamagata K, et al. “Design of the comprehensive health care system for chronic kidney disease (CKD) based on the individual risk assessment by Specific Health Check. Mortality risk among screened subjects of the specific health check and guidance program in Japan 2008-2012. Clin Exp Nephrol. 2017;21:978-985.
14. Sato Y, Fujimoto S, Konta T, et al. Body Shape Index: Sex-Specific Differences in Predictive Power for All-Cause Mortality in the Japanese Population. PLoS One. 2017;12(5):e0177779.
15. Wakasugi M, Kazama JJ, Narita I, et al. Association between overall lifestyle changes and incidence of proteinuria: a population-based, cohort study. Intern Med. 2017;56 (12):1475-1484.
16. Nishimoto M, Tagawa M, Matsui M, et al. A Prediction Model with Lifestyle in Addition to Previously Known Risk Factors Improves Its Predictive Ability for Cardiovascular Death. Sci Rep. 2019;9(1):12953.
17. Wakasugi M, Narita I, Iseki K, et al. The effect of CKD on associations between lifestyle factors and all-cause, cancer, and cardiovascular mortality: a population-based cohort study in Japan. Int Med (in press).
18. Iseki K, Konta T, Asahi K, et al. “Design of the comprehensive health care system for chronic kidney disease (CKD) based on the individual risk assessment by Specific Health Check.et al. Impact of Metabolic Syndrome on Mortality Rate among Participants in Specific Health Check and Guidance Program in Japan. Int Med. 2020;59(21):2671-2678.
19. Nakao YM, Miyamoto Y, Ueshima K, et al. Effectiveness of nationwide screening and lifestyle intervention for abdominal obesity and cardiometabolic risks in Japan: The metabolic syndrome and comprehensive lifestyle intervention study on nationwide database in Japan (MetS ACTION-J study). PLoS One. 2018;13(1):e0190862.
20. Goryoda S, Nishi N, Hozawa A, et al. Differences in Lifestyle Improvements With the Intention to Prevent Cardiovascular Diseases by Socioeconomic Status in a Representative Japanese Population: NIPPON DATA2010. J Epidemiol. 2018;28 Suppl 3(Suppl 3):S35-S39.
21. Hattori T, Konno S, Munakata M. Gender Differences in Lifestyle Factors Associated with Metabolic Syndrome and Preliminary Metabolic Syndrome in the General Population: The Watari Study. Intern Med. 2017;56(17):2253-2259.
22. Sumiyoshi H, Ohyama Y, Imai K, et al. Association of Uric Acid with Incident Metabolic Syndrome in a Japanese General Population. Int Heart J. 2019;60(4):830-835.
23. Takayama S, Takase H, Tanaka T, et al. Smoking Cessation without Educational Instruction could Promote the Development of Metabolic Syndrome. J Atheroscler Thromb. 2018 ;25(1):90-97.
24. Andrés Díaz-López, Nerea Becerra-Tomás, Verónica Ruiz, et al. Effect of an Intensive Weight-Loss Lifestyle Intervention on Kidney Function: A Randomized Controlled Trial. Am J Nephrol. 2021;52(1):45-58.
25. Yamagata K, Makino H, Iseki K, et al. Frontier of Renal Outcome Modifications in Japan (FROM-J). Effect of Behavior Modification on Outcome in Early- to Moderate-Stage Chronic Kidney Disease: A Cluster-Randomized Trial. PLoS One. 2016;11(3):e0151422.
26. Kondo M, Yamagata K, Hoshi SL, et al. Validation of Urine Examination as a Universal Screening. Cost-effectiveness of chronic kidney disease mass screening test in Japan. Clin Exp Nephrol. 2012;16:279-291.
27. Kondo M, Yamagata K, Hoshi SL, et al. Budget impact analysis of chronic kidney disease mass screening test in Japan. Clin Exp Nephrol. 2014;18(6): 885-891.
28. Alkerwi A, Boutsen M, Vaillant M, et al. Alcohol consumption and the prevalence of metabolic syndrome: a meta-analysis of observational studies. Atherosclerosis. 2009;204(2):624-635.
29. Pimenta AM, Lahortiga-Ramos F, Sayon-Orea C, et al. Depression and metabolic syndrome in participants of the "Seguimiento Universidad de Navarra" (SUN) cohort study. J Affect Disord. 2021;284:183-189.
30. Xie J, Li Y, Zhang Y, et al. Sleep duration and metabolic syndrome: An updated systematic review and meta-analysis. Review Sleep Med Rev. 2021;59:101451.
Received: May 5, 2022;
Accepted: May 23, 2022;
Published: May 26, 2022 .
To cite this article : Iseki K, Konta T, Asahi K, Fujimoto S, et al. Virtual Horticultural Therapy: A Qualitative Study Capturing University Students’ Perspectives on Benefits, Challenges and Future Issues. Health Education and Public Health. 2022; 5(2): 496-502. doi: 10.31488/ HEPH.177.
© 2022 Iseki K, et al.
