Research Article / Open Access
DOI: 10.31488/HEPH.189
Multidisciplinary Hearing Rehabilitation and Quality of Life?
Yasmine BOUALLOUCHE, Laura NEROCAN, Dr. Pierre SAFAR
1. Hôpital Sainte Marie Paris, 167, rue Raymond Losserand, France
*Corresponding author:Dr. Pierre SAFAR, Hôpital Sainte Marie Paris, 167, rue Raymond Losserand, 75014 Paris, France, Tel : 01 53 90 63 82
Abstract
To evaluate the impact of multidisciplinary rehabilitation on the quality of life of hearing-impaired adults with hearing aids. Material and Methods : 23 patients with acquired hearing loss acquired with hearing aids benefited from multidisciplinary rehabilitation in part-time hospitalization. This 5-week program, 2 half-days per week with 2 sessions per half-day, included: speech therapy, occupational therapy, psychomotor skills, psychology and social monitoring. Quality of life was assessed by the ERSA self-questionnaire at entry and exit from the rehabilitation course. To improve the care of hearing-impaired patients with hearing aids whose follow-up after the fitting of hearing aids is often limited, sometimes leaving deprived patients who underuse or even abandon the devices. 23 subjects benefited from the multidisciplinary hearing rehabilitation program. Overall quality of life improved significantly for 20 patients (87%). The improvement in quality of life is significant, regardless of professional activity, age or degree of severity of deafness up to a total of 29 sessions. Beyond 29 sessions, we did not measure any significant improvement in quality of life scores. A multidisciplinary hearing rehabilitation course for hearing-impaired patients significantly improves ERSA quality of life scores up to a total of 29 sessions. These encouraging results need to be confirmed at a distance from the rehabilitation course to ensure medium-term benefit and in larger populations with a control group to limit bias.
Keywords: Hearing loss, quality of life, Aural multidisciplinary rehabilitation, hearing impairment habilitation
Introduction
In 2008, the Handicap-Santé survey recorded 10 million people with hearing impairments in France, representing 16% of the population. Among them, 5.4 million had moderate to profound hearing impairments that affected their daily lives. [1,2]. In 2010, in France, of the 600,000 people with hearing loss using hearing aids [1,2], 360,000 (60%) had severe to total activity limitations and were unable to follow a conversation involving several people [2]. Hearing impairments can lead to activity limitations, such as difficulty understanding in noisy environments or among multiple speakers, as well as cognitive decline [3-5].
They restrict communication, the quality of interactions, the intake of information from the environment, personal and professional fulfillment, and social relationships, with a risk of isolation [6][2]. There are also psychological well-being consequences [7]. A study by Chuan-Ming L. et al. shows that individuals with even mild hearing impairments suffer from moderate to severe depression in 11% of cases, compared to just 5% in the general hearing population [8]. The quality-of-life indicators (psychological distress, access to healthcare, isolation, communication) for individuals with hearing impairments are therefore much poorer compared to the general population [6,2]. The adaptation of hearing aids by an audiologist is a critical step in the management of hearing impairments [9,10]. However, a survey conducted by INSEE between 1998 and 2001 highlighted that only 40% of hearing aid users were satisfied with their devices [11].
If hearing aids are insufficient, auditory rehabilitation and learning lip-reading with a speech therapist may be offered [11-13]. These interventions target auditory-cognitive dimensions [14] without considering the functional, psychological, social consequences, or their real-world implications [7].
Does a multidisciplinary rehabilitation program improve the overall quality of life of patients by addressing all their impairments [14]. We did not find any studies in the literature on a multidisciplinary rehabilitation approach addressing all the impacts of hearing impairments in France [14-15].
The aim of this study is to evaluate the impact of a multidisciplinary auditory rehabilitation program on the quality of life of adult patients using hearing aids with mild to profound hearing loss.
To measure the consequences of a multidisciplinary rehabilitation program, a self-administered quality of life questionnaire, the Evaluation du Retentissement de la Surdité chez l’Adulte (ERSA) [16], is used before and after the treatment program.
Materials and Methods
The study conducted between December 2018 and June 2021 included 23 adult patients with hearing loss, comprising 15 women and 8 men, aged 34 to 81 years. The median age was 64 years, and the mean age was 62.4 years.
These 23 French-speaking subjects all had acquired hearing loss (mild, moderate, severe, or profound) and used hearing aids, without any known cognitive impairments. This study received prior approval from the Medical Ethics Research Group at Saint Joseph Hospital and was published on the Health Data Hub platform (No. F20211201151717).
Each subject participated in a multidisciplinary rehabilitation program on a part-time inpatient basis. The program began with a tonal and speech audiogram, conducted with and without hearing aids under binaural free-field and headphone listening conditions, using masking techniques by an ENT specialist and an audiologist. Advice and recommendations regarding the use of hearing aids were also provided. Audiometric tests (speech audiometry in noise, Hearing in Noise Test, dichotic listening, sound localization, sound identification) and cognitive tests (MoCA, lip reading, fluency tests, Stroop test, visual attention block tests) were administered by a speech therapist. An occupational therapist assessed participation restrictions through a semi-structured interview and evaluated the quality of life before and after rehabilitation using the ERSA self-questionnaire.
The ERSA self-questionnaire is a validated test that evaluates quality of life in the psychological, social, personal, and professional dimensions of individuals with hearing loss. It is divided into four sub-domains: quality of life, personal life, social life, and professional life, each with five questions rated on a 10-point scale. Participants with professional activity have a maximum score of 200 points, while those who are not professionally active are scored out of 150.
Each sub-domain of the test (global quality of life, social life, and personal life) includes aspects of communication with the patient’s surroundings in quiet or noisy environments, both with and without prior knowledge of the topic. The professional life sub-domain includes questions related to meetings, phone use, and the acquisition of new knowledge.
The initial assessment concludes with evaluations by psychomotor therapists, a social worker, and a psychologist to assess the psycho-social-somatic impacts of hearing loss.
All patients underwent at least fifteen rehabilitation sessions. The sessions were distributed over five weeks, with two half-days per week.
Each half-day included at least two individual sessions in different domains: speech therapy, occupational therapy, psychomotricity, or with the psychologist. Each session within a domain was provided by the same therapist throughout the program. The therapists acted both as evaluators and as rehabilitation providers for the patients.
In speech therapy, patients received cognitive training focused on attention skills, executive functions, lip reading, and auditory training in an auditorium for sound localization, low-intensity speech comprehension, understanding in noise, and dichotic listening.
In occupational therapy, rehabilitation focused on analyzing real-life situations to identify barriers to performing activities, recommending compensatory strategies and/or appropriate assistive devices, and providing support for social-professional reintegration.
In psychomotricity, rehabilitation addressed relaxation, tonic regulation, stress management, and balance. One or two real-life simulation sessions focusing on phone use, stress management in noisy environments, or improving comprehension in real-world situations (such as in a café) were organized collaboratively by two professionals from complementary fields, such as occupational therapist, speech therapist, and psychomotrician.
Finally, psychological and social follow-up, with one to two sessions per patient, was offered during the rehabilitation program.
At the end of the rehabilitation program, a final comparative evaluation was conducted.
Our primary evaluation criterion for assessing the impact of the multidisciplinary rehabilitation on patients with hearing loss who use hearing aids is the comparison of the ERSA score before and after rehabilitation.
Results
Twenty-three patients, 15 women (65%) and 8 men (35%), benefited from the multidisciplinary rehabilitation program.
Four patients had mild hearing loss (17%), seven had moderate first-degree hearing loss (30%), eight had moderate second-degree hearing loss (36%), one had severe first-degree hearing loss (4%), two had severe second-degree hearing loss (9%), and one had profound hearing loss (4%). The most common degree of hearing loss in our sample was moderate. Among all the patients included in this study, thirteen patients were professionally or socially active (52%), and ten were not (48%). The ERSA score significantly increased in 20 out of 23 patients, or 87% of the total population. The interpretation of the results, based on the work of E. Ambert-Dahan et al. [16], highlights a significance threshold of +6 +/- 11.0 for ERSA results on 150 points for the group without professional activity, and +4 +/- 13.3 for results on 200 points for the group with professional activity [16]. Of the 23 patients, one maintained their initial quality of life, and two noted a non-significant decrease in their quality of life. A significant increase of 25.5 points out of 200 was found in the group with professional activity (Figure 1); and a suggestive increase of 15.45 points out of 150 was observed in the group without professional activity (Figure 2).
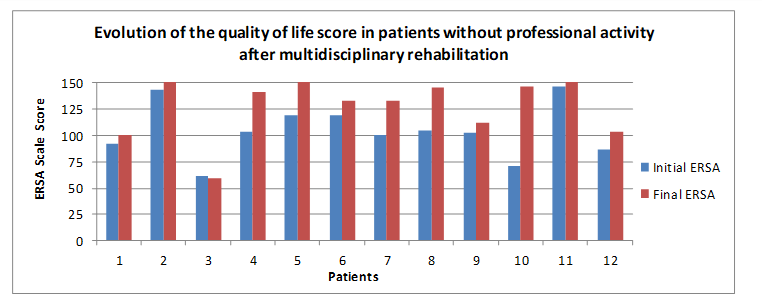
Figure 1: Evolution of the quality of life score in patients without professional activity after multidisciplinary rehabilitation.
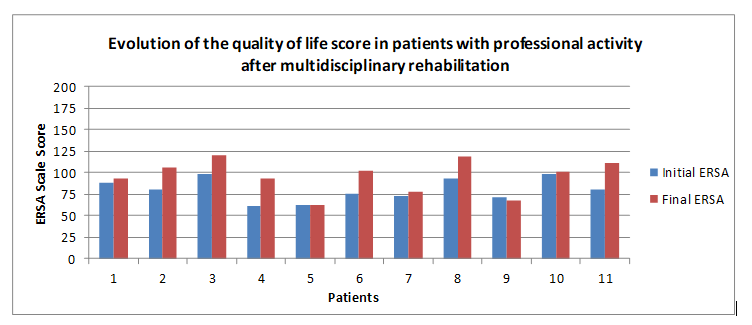
Figure 2:Evolution of the quality-of-life score in patients with professional activity after multidisciplinary rehabilitation.
Thus, all the subdomains assessed by the ERSA showed significant improvement. Among these four subdomains, the increase was 5.13 points out of 50 (p=0.0001) for the quality-of-life item, 6.82 out of 50 (p<0.0001) for the personal life item, 4.95 out of 50 (p=0.002) for the social life item, and 6.58 out of 50 (p=0.006) for the professional life item (Fig. 3). The multidisciplinary rehabilitation appears to have had a favorable impact, with an average increase of 6.82 points for personal life and a comparable result in the professional life domain of 6.58 points (Fig. 3).
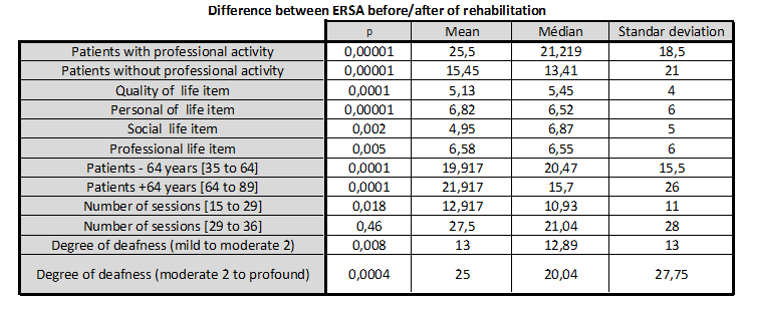
Figure 3:Analysis Table of ERSA Results. A preliminary Shapiro-Wilk test was conducted to ensure that our patient population followed a normal distribution. To analyze the results, a Student's t-test was performed.
An increase in ERSA scores was also observed across the entire population, regardless of the patient's age ([35-64 years] p = 0.0001; [64-89 years] p = 0.0001) (Figure 3). There was a significant increase of 25.5 points (p=0.0004) in the group from moderate second-degree hearing loss to profound hearing loss, and a suggestive increase of 13 points (p = 0.008) in the group from mild to moderate second-degree hearing loss. Multidisciplinary rehabilitation thus appears to be beneficial, regardless of the severity of the hearing impairment.
All patients received between 15 and 36 rehabilitation sessions. Two subgroups were formed based on the median number of sessions performed (29 sessions). Patients who received fewer than 29 sessions showed a suggestive increase of 27.5 points (p=0.018) in the ERSA self-questionnaire. Patients who received more than 29 sessions showed a non-significant increase of 12.9 points (p=0.469). The group of patients who completed more than 29 sessions did not seem to experience a better overall quality of life than the group who participated in fewer than 29 sessions.
Discussion
A study was carried out on the impact of multidisciplinary rehabilitation on the quality of life of patients with hearing aids. The results, based on the analysis of the ERSA self-questionnaire, showed that multidisciplinary rehabilitation significantly improved the overall quality of life of patients (total result of the ERSA test).
As a reminder, ERSA evaluates different aspects of life such as quality of life, personal life, social life and professional life. The results showed that each aspect was improved by multidisciplinary rehabilitation. Furthermore, the rehabilitation pathway also improves quality scores in all patients, regardless of their degree of deafness. However, the benefit remains greater in patients with “moderate 2 to profound” hearing loss. The study also showed that the rehabilitation course was beneficial for patients of all ages. Also, the rehabilitation course proved to be effective over a relatively short rehabilitation period, up to 29 sessions. The improvement in quality of life seemed insignificant beyond the recommended 29 sessions.
Finally, the impact of hearing rehabilitation was greater in patients with a professional activity than those without. Also, in the study of the ERSA results, we note that the “personal life” scores represented the most significant benefit felt by patients.
Given the patients' main initial complaint, particularly focused on understanding in noise and multi-speaker conversation, it was subjectively proven that at the end of their rehabilitation, patients described greater ease and confidence in initiating a conversation. With their loved ones as well as participating in multi-speaker meetings.
However, we can question the influence of joint sessions led by several professionals: Do they particularly favor the increase in the four sub-domains of ERSA? It would be interesting in a future study to compare the evolution of quality of life with objective assessments of hearing-cognitive abilities.
In addition, we can note several biases in this study. The small population studied does not allow for an in-depth statistical analysis. To the same extent, the absence of randomization and a control group limits the interpretation of the results. Additionally, the fact that the rehabilitators and evaluators are the same people may constitute another measurement bias. Finally, an evaluation at 6 months would make it possible to determine whether the improvement in quality of life is maintained in the medium term. Furthermore, several biases can be noted in this study. The small sample size does not allow for in-depth statistical analysis. Similarly, the lack of randomization and a control group limits the interpretation of the results. Additionally, the fact that the rehabilitation providers and evaluators were not distinct from one another constitutes a measurement bias, as well as biases in interpretation and test reproducibility. Finally, a follow-up assessment at 6 months would help determine whether the improvement in quality of life is maintained in the medium term.
Conclusion
This study on 23 patients is an initial contribution in favor of multidisciplinary auditory rehabilitation for adults with hearing impairments who use hearing aids.
All the sub-domains evaluated by the ERSA were significantly improved, regardless of the patients' age, degree of hearing loss, or professional status, indicating a significant increase in their quality of life.
The items related to professional and personal quality of life were the ones that most benefited our patient population.
The results revealed a suggestive benefit only when patients participated in fewer than 29 sessions. Should the duration of the program be considered, or was the population too heterogeneous and the sample too small to demonstrate a benefit?
These encouraging results, however, need to be moderated and confirmed by further studies on a larger, randomized population with a control group. Additionally, an objective assessment focused on auditory-cognitive functions would help correlate the subjective data obtained. Finally, analyzing the ERSA data by sub-domains would provide further insights into which population benefits the most from multidisciplinary auditory rehabilitation.
Abbreviations
INSEE : Institut national de la statistique et des études économiques; ERSA : Evaluation du Retentissement de la Surdité chez l’Adulte ; ENT Ear and Nose and Throat ; MoCA Montreal Cognitive Assessment
Conflicts of Interest
The authors declare that they have no conflicts of interest to disclose. This research received no specific funding from public, commercial, or nonprofit funding agencies. The data can be shared publicly.
Acknowledgments
The authors would like to thank all the patients as well as the Sainte Marie Hospital in Paris for their significant contribution to this study.
References
1. Ministère du Travail, des Relations Sociales, de la Famille, de la Solidarité et de la Ville & Secrétariat d’État chargé de la Famille et de la Solidarité. Plan 2010-2012 en faveur des personnes sourdes ou malentendantes. 2010. Available from: https://www.cnsa.fr/documentation/plan_en_faveur_des_personnes_sourdes_ou_malentendantes_-_10_02_2010.pdf
2. Bucodes SurdiFrance. Publication du livre Baromètre Santé Sourds et Malentendants. Available from: https://surdifrance.org/127-articles-archives/archives-articles-2016/310-publication-du-livre-barometre-sante-sourds-et-malentendants
3. Brodie A, Smith B, Ray J. The impact of rehabilitation on quality of life after hearing loss: a systematic review. Eur Arch Otorhinolaryngol. 2018 Oct;275(10):2435-2440.
4. Golub JS, Brickman AM, Ciarleglio AJ, Schupf N, Luchsinger JA. Association of Subclinical Hearing Loss With Cognitive Performance. JAMA Otolaryngol Neck Surg. 2020 Jan;146(1):57.
5. Leusie S. Privation sensorielle auditive et réhabilitation chez le sujet âgé : conséquences sur le fonctionnement cognitif [thesis]. Lyon 1; 2015. Available from: https://www.theses.fr/2015LYO10043
6. Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life of elderly adults. Clin Interv Aging. 2012;7:159-163.
7. Haeusler L. Étude quantitative sur le handicap auditif à partir de l’enquête « Handicap-santé ». 2008;156.
8. Li CM, Zhang X, Hoffman HJ, Cotch MF, Themann CL, Wilson MR. Hearing Impairment Associated With Depression in US Adults, National Health and Nutrition Examination Survey 2005-2010. J Am Acad Audiol. 2014;10:1-7.
9. Guevara N, Lina-Granade G, Seldran F, Truy E, Gallego S. L’implant cochléaire en 2015. Pour qui? Pour quoi? ORL Autrem. 2015 Jan;1:1-5.
10. Maidment DW, Barker AB, Xia J, Ferguson MA. Effectiveness of alternative listening devices to conventional hearing aids for adults with hearing loss: a systematic review protocol. BMJ Open. 2016 Oct;6(10):e011683.
11. Ernst É. Quelle est la place de l’orthophonie dans le traitement de la surdité? 1997;1.
12. Bonvarlet M. La rééducation orthophonique des adultes presbyacousiques. 1999;88.
13. Cailleteau C. Intérêt de l’intervention orthophonique auprès d’adultes devenus sourds en difficulté d’adaptation prothétique. Audiol Direct. 2020;(4):1.
14. Oberg M, Bohn T, Larsson U, Hickson L. A preliminary evaluation of the active communication education program in a sample of 87-year-old hearing impaired individuals. J Am Acad Audiol. 2014 Feb;25(2):219-228.
15. Beche C. Presbyacousie: le parcours de soins du patient appareillé: enquête sur la ville de Nancy et son agglomération. 2009;81.
16. Ambert-Dahan E, Laouénan C, Lebredonchel M, Borel S, Carillo C, Bouccara D, et al. Évaluation du retentissement de la surdité chez l’adulte: validation d’un questionnaire de qualité de vie. Ann Fr Oto-Rhino-Laryngol Pathol Cervico-Faciale. 2018 Feb;135(1):29-35.
Received: January 07, 2025;
Accepted: January 29, 2025;
Published:January 31, 2025 .
To cite this article : BOUALLOUCHE Y, NEROCAN L, SAFAR P. Revolutionising participants health and wellbeing through neuro-reprogramming by using breakthrough research in "nudge" thinking to retrain habitual and emotional responses to foodstuffs. Health Education and Public Health. 2025; 8(1): 571-574. doi: 10.31488/HEPH.189.
© The Author(s) 2025. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/).
